Narrowing the Gap: New Device Makes Heart Valve Repair Safer, Easier
Date
March 22, 2022
Credits
Date
March 22, 2022
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Most patients with pulmonary valve disease may avoid open-heart surgery to have their valves repaired, thanks to a new device pioneered at Cedars-Sinai and recently approved by the Food and Drug Administration (FDA).
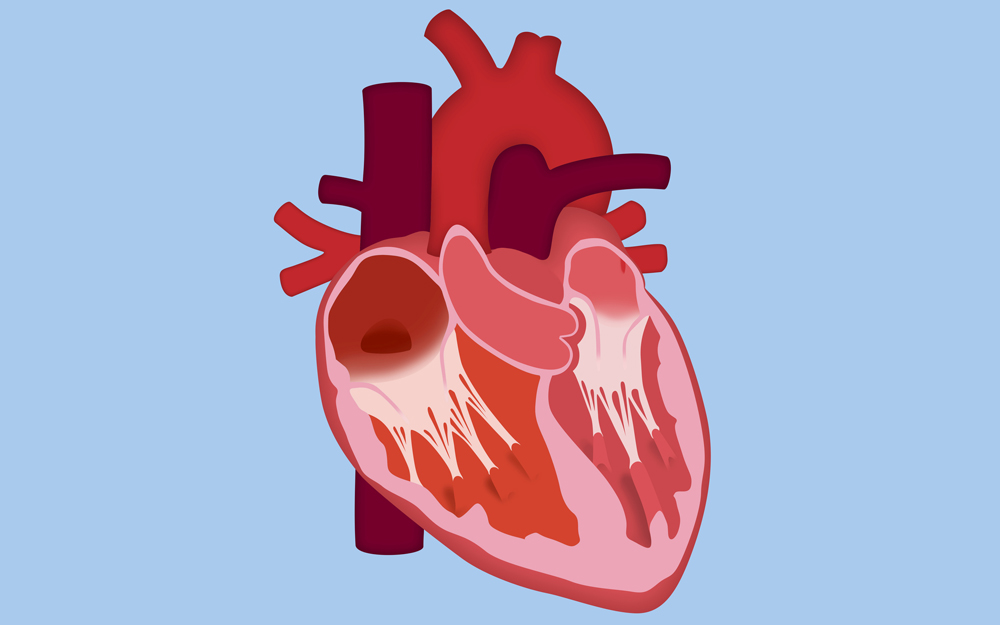
The pulmonary valve controls blood flow from the heart to the lungs. The valve can malfunction in a number of ways. Conducting pulmonary valve repair using a minimally invasive procedure should improve patients’ quality of life and significantly shorten their recovery time, compared to open procedures.
"We came up with a concept to try to reshape that pulmonary valve area and make it something that was amenable to simple valves, and we actually did a small series of cases here using a device we made. We’re very MacGyver-oriented in our subspecialty."
"Even with surgery being as good as it is these days, you’re still looking at a five- to seven-day hospitalization in an intensive care unit, and your chest takes six weeks to heal," says Dr. Evan Zahn, director of the Congenital Heart Program at Cedars-Sinai. "With the new device, you’re talking about 23 hours in the hospital and a Band-Aid on the surgery site, and you go home the next day. It’s quite a difference."
When someone is born with pulmonary valve disease, they typically need several open-heart surgeries over the course of their lifetime to repair and replace the faulty heart valve. About 1 in 2,000 babies is born with the condition.
Twelve years ago, the FDA approved a pulmonary heart valve that could be inserted via catheter, which reduced the number of lifetime open-heart surgeries for some people. However, only 10% to 15% of patients with pulmonary valve disease were eligible for this valve—the majority still needed open-heart surgery.
"The problem was, for the vast majority of patients, that area that you’re trying to put a valve in is, number one, too irregularly shaped, and number two, just simply too big," Dr. Zahn says.
The new device, known as the Alterra pre-stent, solves this problem for up to 80% of patients. It’s shaped like an hourglass, which simultaneously fills and reduces the size of a larger space. It’s also designed to standardize the shape of the pulmonary valve opening, so that a valve can easily be placed within it.
During a minimally invasive procedure, a catheter is threaded through a blood vessel in the leg until it reaches the heart, where the device is positioned and implanted, along with a replacement heart valve. Once implanted, the pre-stent becomes a permanent structure within the heart.
The valve, however, may ultimately need to be replaced. When someone needs a new pulmonary valve, the replacement may be implanted again by catheter within the pre-stent, which has a large enough space to accommodate several valves, potentially eliminating future open-heart surgeries.
"Like a Russian doll, you can just keep putting new ones inside of the pre-stent using catheterization," Dr. Zahn says. "The new device is intended to minimize or eliminate the number of surgeries that someone would need."
Engineering a Solution
In 2012, Dr. Zahn and colleagues decided to create a device that could be inserted by catheter to modify the pulmonary valve space so that a standard-sized valve could fit.
"We came up with a concept to try to reshape that pulmonary valve area and make it something that was amenable to simple valves, and we actually did a small series of cases here using a device we made," Dr. Zahn says. "We’re very MacGyver-oriented in our subspecialty."
Once Dr. Zahn and colleagues successfully performed minimally invasive surgery to implant their uniquely designed devices in several patients with pulmonary valve disease, they decided to collaborate with Edwards Lifesciences, which makes devices to correct structural heart problems.
"Their engineers came up with this concept, which basically does what we were doing, but in a much more elegant and user-friendly and predictable way," Dr. Zahn says.
Dr. Zahn was named principal investigator of clinical trials for the Alterra device, and in 2017, he implanted the world's first Alterra pre-stent in a patient. That woman recently had her five-year checkup, and she's doing well. After the FDA approved the device in December 2021, Dr. Zahn successfully implanted the world's first commercially available Alterra pre-stent in a patient in January 2022.
Between 70% and 80% of adults, teens and elementary-school-aged children with pulmonary valve disease may now opt for this minimally invasive procedure instead of undergoing open-heart surgery, but Dr. Zahn won't be satisfied until a similar device can be implanted in the tiniest patients.
Infants with pulmonary valve disease may need open-heart surgery when they're just 3 or 6 months old. For years, Dr. Zahn has been working to create a stent that could be placed via minimally invasive surgery into a baby's pulmonary artery, then remain there through adulthood, eliminating the need for open-heart surgeries in the future. He's helped design the Minima stent—what he calls the "Holy Grail stent"—which is in clinical trials now. Cedars-Sinai is one of four study sites.
"That's going to change everything, I think," Dr. Zahn says.