Getting the Diagnosis Right With Multiple Sclerosis
Date
April 11, 2022

Date
April 11, 2022
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Nearly one in five patients with an established diagnosis of multiple sclerosis (MS) are misdiagnosed, according to a 2019 study led by Cedars-Sinai.
"Many physicians think diagnosing MS is simple," Marwa Kaisey, MD, one of the study's lead authors, said. "We need more education on why it's not and how people get the diagnosis wrong."
Kaisey and her colleague Omar Al-Louzi, MD, are both MS specialists at Cedars-Sinai. In collaboration with researchers and experts across the medical center, the pair of neurologists are at the forefront of developing new tools and techniques to improve the efficiency and accuracy of MS diagnoses.
"A big problem in MS is we have a lot of tools that detect everyone who may have MS but also lump in people with other conditions that are not MS," Kaisey said. "We don't yet have tools that will identify only MS. We have sensitive markers but not specific markers to distinguish MS from other diagnoses."
"Sometimes, patients who are misdiagnosed with MS are placed on MS therapies that alter or suppress the immune system. This can put patients who don't have MS at a higher risk of side effects, including infection."
The danger of misdiagnosis
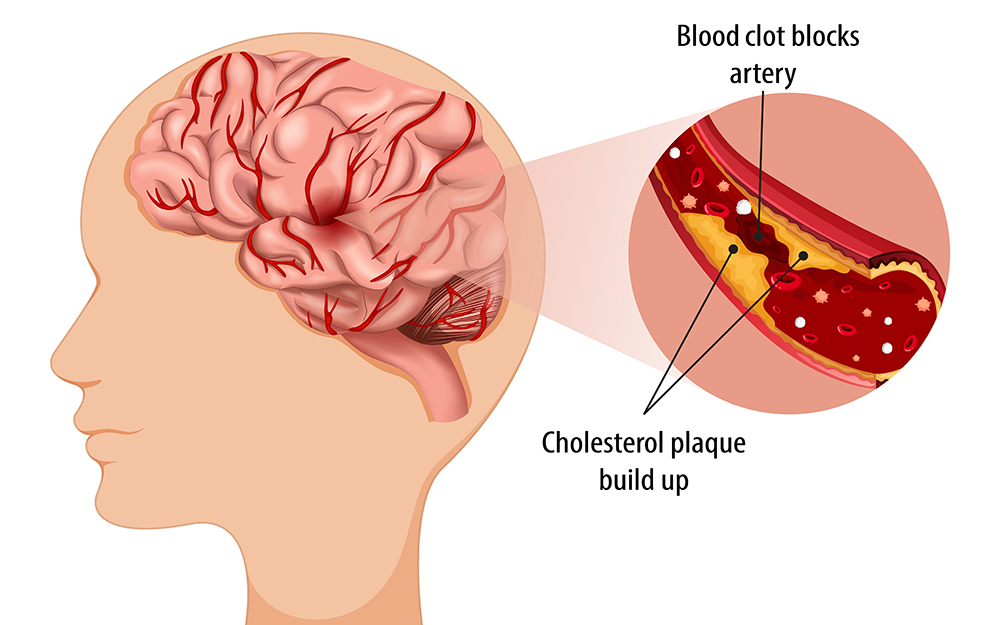
To diagnose MS, physicians first obtain a thorough history to understand a patient's symptoms—particularly whether symptoms are experienced as discrete attacks or are slowly progressing over time. Then, a physical exam is conducted to understand inflammation in the brain, spinal cord and optic nerves. MRI is used to look for the presence of lesions in particular compartments of the brain and spinal cord.
Even with all these diagnostic criteria, many neurological conditions can masquerade as MS, and vice versa. Migraine is commonly confused with MS, as are other medical conditions such as cerebral small vessel disease, systemic lupus erythematosus, or autoimmune conditions like neuromyelitis optica or myelin oligodendrocyte glycoprotein antibody-associated disease. For all these conditions, the lesions on the brain MRI can present similarly.
"People often come into our clinic with an abnormal brain MRI, and no one knows what's causing their lesions," Kaisey said.
Misdiagnosis holds critical consequences for patients' health, which is why the Cedars MS and Neuroimmunology program, led by Nancy Sicotte, MD, has been focused on developing and utilizing novel diagnostic biomarkers.
"Sometimes, patients who are misdiagnosed with MS are placed on MS therapies that alter or suppress the immune system," Sicotte said. "This can put patients who don't have MS at a higher risk of side effects, including infection." This can be particularly dangerous for patients who have an autoimmune condition that does not respond to these medications.
On the other hand, the risks are also great for patients who truly do have MS but are misdiagnosed with a different, mimicking condition. A delay in proper MS treatment can increase the risk of relapses, intensified or new symptoms, and disability down the road.
"The main risk is that the disease goes on to be uncontrolled for longer when it doesn't have to be," Al-Louzi said. "If we were accurate in diagnosing it early, we can initiate effective therapies that match the patient's risk profile and effectively control the disease."
Advanced MRI technology
Given these challenges to accurate, early diagnosis, researchers at Cedars-Sinai are focused on developing new, more precise diagnostic tools targeting MS.
The first is a biomarker called the central vein sign. It's an MRI finding that can allow for higher-resolution imaging and identification of veins and venules. This imaging technique can help determine whether a patient's brain lesions form around small blood vessels—a feature that distinguishes MS from other conditions.
"This marker of whether lesions develop around veins and venules in the brain is highly specific for MS, and it can help us confirm the diagnosis compared to other conventional methods," Al-Louzi said.
Several single-center studies and retrospective analyses have been published on the central vein sign. In partnership with the National Institutes of Health, Cedars-Sinai is currently recruiting 400 patients throughout the country for a multicenter study that utilizes the central vein sign when diagnosis is still unclear and then follows the patients for two years.
Further research is underway to examine whether the use of gadolinium could enhance the visibility of these particular veins and venules on an MRI scan. Researchers are also looking at ways to leverage artificial intelligence to make the advanced imaging more accessible for community use outside the academic medical center setting.
Another biomarker that is promising in advancing MS diagnosis is paramagnetic rim lesions, which are thought to represent lesions in MS with evidence of chronic active inflammation.
Traditionally, the accumulation of iron at the edge of these lesions has indicated a higher risk of developing severe MS that leads to disability or more frequent inflammatory breakthroughs.
Emerging research is evaluating whether these paramagnetic rim lesions can help diagnose MS earlier.
"We're seeing very encouraging data that the presence of those lesions at the initial scan can help us make a diagnosis of MS when combined with other clinical and radiological features," Al-Louzi said.
Yet another diagnostic tool being explored at Cedars-Sinai is the use of blood biomarkers connected to MS. Alongside expert partners in experimental proteomics, Kaisey is in the early stages of investigating this cutting-edge technique.
"We're looking at whether there are proteins or parts of proteins in our blood that can give us a look into what's going on in the central nervous system itself." Kaisey said. "Until now, we didn't have sensitive enough technology to pick up the small proteins that make it from the spinal fluid into the blood."
Securing a blood sample is much easier and less invasive for patients compared to a spinal tap and lumbar puncture.
Engaging MS specialists
Given the challenges of diagnosing MS, the prevalence of mimicking conditions and the constantly evolving diagnostic criteria, Kaisey and Al-Louzi recommend that patients who have MS or are newly diagnosed with MS see a specialist at least once to confirm their diagnosis and obtain an initial evaluation about a treatment strategy.
Cedars-Sinai's subspecialized MS experts have access to cutting-edge diagnostic tools, and when it comes to treatment, they are well-versed in the full spectrum of approved MS medications and their safety profiles, including infusions.
"We can help make sure that the diagnosis is accurate, and we can help develop a treatment strategy that is tailored to each patient and keeps risks to a minimum," Al-Louzi said.