The Brain's Social Networks
Date
July 2, 2025
Credits

Date
July 2, 2025
Credits
Medical providers featured in this article

In Brief
{{cta-block}}
Social connections—and how we feel about them—are closely interwoven with our brains’ own networks.
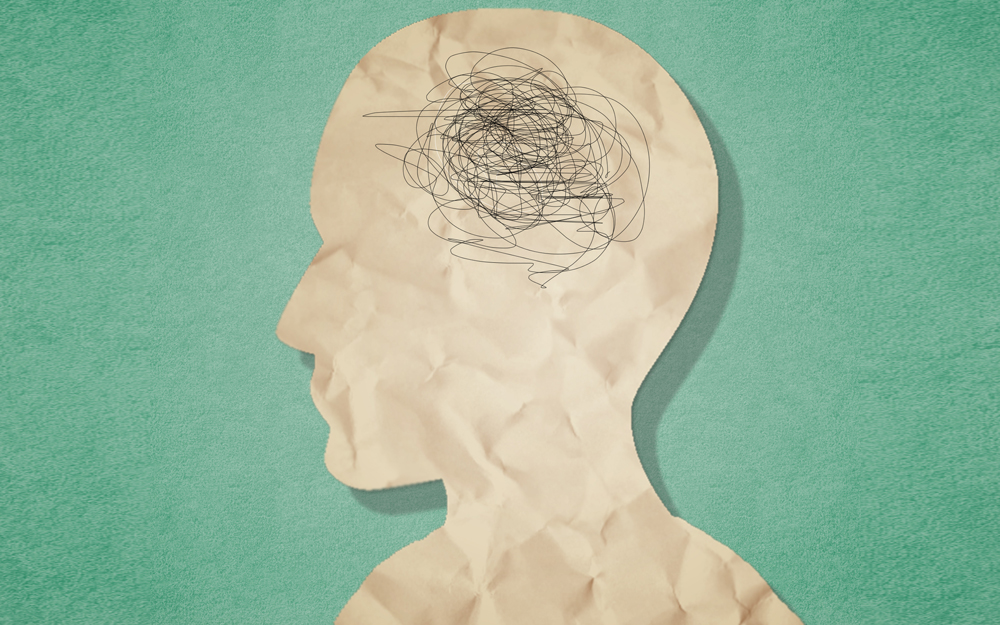
Increasing evidence underscores the integral relationship between loneliness, social isolation and dementia. In a 2022 retrospective analysis of Framingham Heart Study data, Cedars-Sinai neuropsychologist Mitzi Gonzales, PhD, and co-investigators found study participants who were not genetically predisposed to dementia were three times more likely than peers to develop the disease in the next decade if they reported loneliness. Even those with occasional loneliness—three days in a week—had increased risk.
Social isolation, another growing concern among approximately one-quarter of older U.S. adults aging in place, can increase a person’s vulnerability for dementia by up to 50%.
In a post-pandemic, technologically advanced world, people are more physically distanced yet digitally attached—and investigators at Cedars-Sinai and across the country are collaborating to untangle these complex links.
“We are missing data to fully characterize the scale and magnitude of loneliness,” said Gonzales, director of Translational Research at the Jona Goldrich Center for Alzheimer’s and Memory Disorders at Cedars-Sinai. “It is essential to understand what is happening in the brain in light of these shifts in how we connect.”
Support Networks
In animal models, solitary living has been linked to brain inflammation, protein plaque accumulation and potentially destabilizing oxidative stress, as well as the erosion of vital neuron connections.
Gonzales and partners at the NYU Grossman School of Medicine (led by Joel Salinas, MD) and Boston University Chobanian and Avedisian School of Medicine seek to determine the mechanisms driving the associations across a wide range of social experiences, health statuses and ages. Using novel brain imaging and machine learning, they are analyzing over 70 years of data from the same Framingham Heart Study multigenerational cohort.
“We always face this chicken-and-egg scenario: Is it that people are developing pathology in their brain that affects their behavior and causes them to withdraw,” Gonzales said, “or could disconnection happen first and potentially play a role in propagating the neurodegenerative disease pathology?”
As humans, we’re wired to seek connection. We’re not meant to be by ourselves.”
— Allison Mays, MD
In their 2022 study, Gonzales and partner investigators found that study participants who didn’t develop dementia but reported loneliness still exhibited Alzheimer’s disease biomarkers, including a larger burden of white matter lesions and reduced brain volume and executive function.
The researchers will further explore brain structure and blood samples alongside measures of loneliness, social networks and cognition, including executive and visuo-spatial functioning, learning, and memory. Often, these are the first skills compromised by neurodegenerative disease. The study could reveal inflammatory, vascular or other cognitive pathways, shedding new light on their effects alone and in tandem.
Moving Through Time
While the value of community is becoming apparent, its shape is constantly evolving.
Such fluctuations in society and methods of interaction strain the ability to measure social engagement accurately, Gonzales said. The new analysis aims to compensate by drawing on a large sample size of more than 15,000 participants over a vast timespan.
For insight into socialization, investigators are focused on the number of close relationships a person has and their frequency of different types of contact. Changes in executive skills could also be a useful window, since maintaining connections and gathering with adult peers, friends and relatives requires considerable organization.
Though nearly half of U.S. adults aged 60 and older report loneliness—an internal perception—not all are isolated.
“Social engagement and loneliness are interrelated, but not the same,” Gonzales said.
Future research will seek to pinpoint whether broad generational shifts in social behavior, such as the advent of social media or women moving into the workforce, alter brain aging.
Risk Calculations
Across a burgeoning research focus, Cedars-Sinai’s aging experts are carefully unraveling drivers of Alzheimer’s and dementia and developing personalized prevention approaches.
Robust relationships may be protective, representing a vital opportunity for the swelling population of older Americans who are most vulnerable.
“As humans, we’re wired to seek connection,” said Cedars-Sinai geriatrician Allison Mays, MD, whose Leveraging Exercise to Age in Place (LEAP) study led to the establishment of Cedars-Sinai’s Forever Fit community program. “We’re not meant to be by ourselves.”
Experts are weighing social habits with age and genetic and environmental risks, such as neighborhood access to public spaces, to determine who might be most vulnerable to loneliness. Ultimately, they are pursuing individual and societal interventions.
“There could be a critical period for socialization, such as when you are young and developing or as you age, lose loved ones and are more likely to live alone,” Gonzales said. “Conversely, community could be more like a garden we have to nurture and shape for the rest of our lives.”