A Double-Edged Sword: Inflammation and Your Health
Date
February 12, 2021
Credits

Date
February 12, 2021
Credits
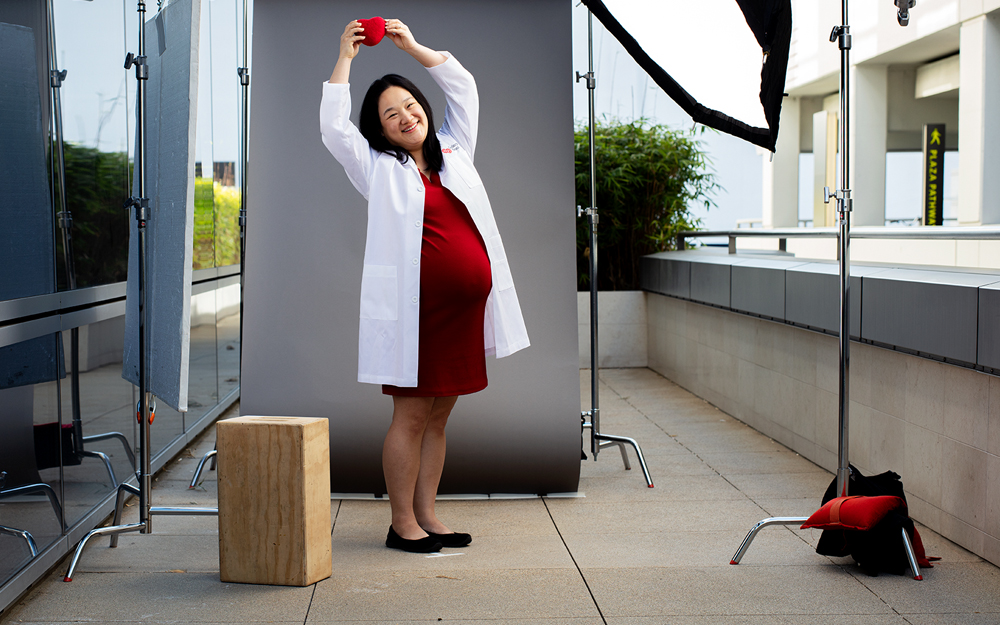
Medical providers featured in this article
In Brief
{{cta-block}}
It’s March 2020. John is experiencing shortness of breath, fatigue and a low-grade fever, and a mysterious loss of his senses of smell and taste. A test reveals he is positive for COVID-19. Within weeks, the otherwise healthy 38-year-old is in the intensive care unit on a ventilator. The infection spins out of control like a tornado, ravaging every organ system in its wake. What propelled that two-month physiological cyclone? Inflammation.
"Inflammation is largely the body's defense mechanism against things that should not be in the body. But as with any complicated defense system, any misstep can lead to friendly fire."
"The most severe cases of COVID-19 seem to develop from an overactive inflammatory response that's kick-started to battle the virus but ultimately overwhelms the body," explains Helen S. Goodridge, PhD, an immunologist at Cedars-Sinai. This so-called cytokine storm continues churning out inflammatory cells, signaling the body to keep going and going and going.
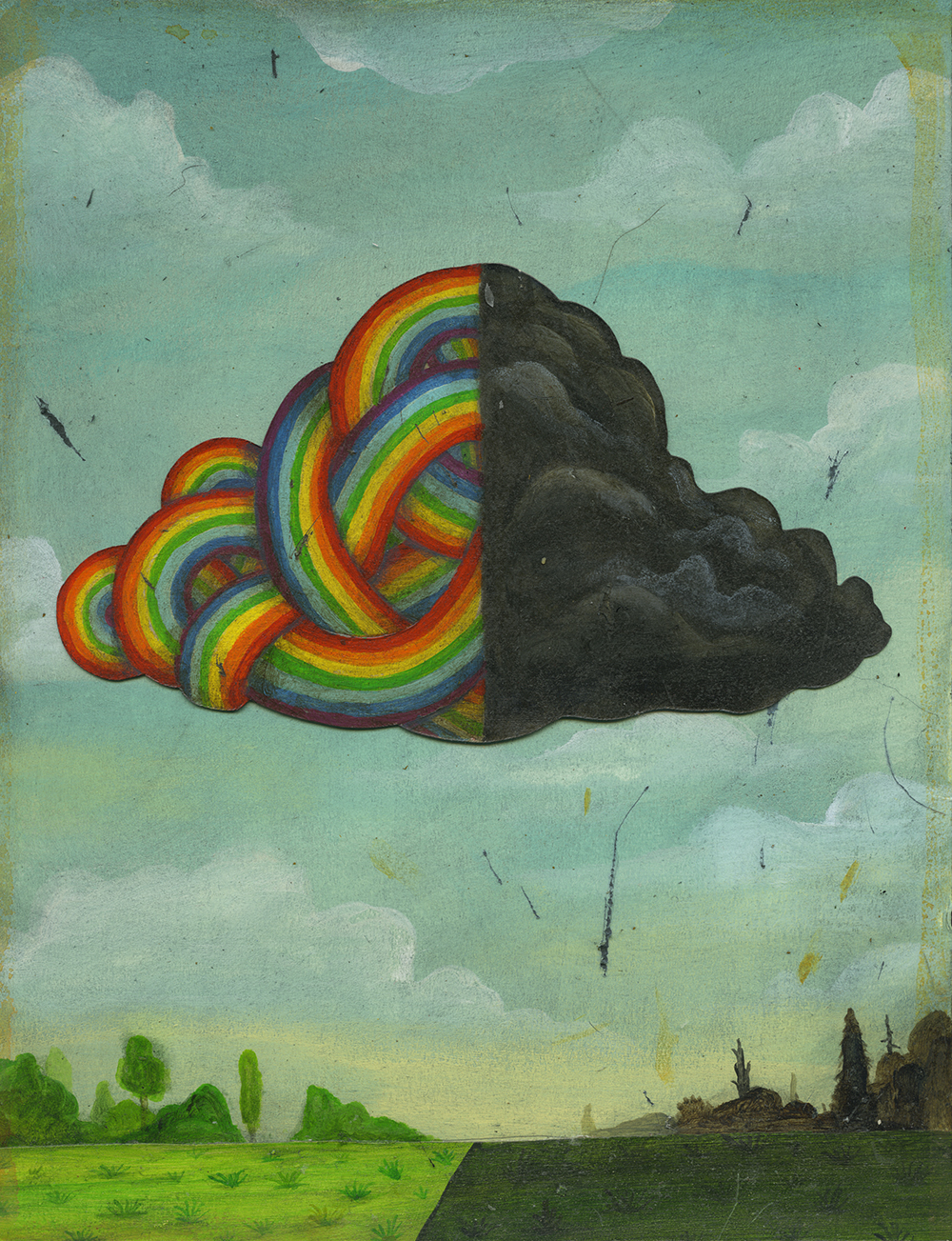
It turns out that COVID-19 is a textbook illustration of how runaway inflammation can drive disease through multiple organ systems. While there are new clues as to why this may be happening with a coronavirus infection (see sidebar, below), what still baffles scientists is how the same inflammatory response that can wipe out an otherwise healthy patient can also play a key role in the recovery of thousands of others.
At the heart of the issue is understanding the beneficial and detrimental roles that inflammation plays in disease processes and using that knowledge to develop targeted treatments—ones that can both incite the inflammatory response and shut it off after the threat has passed.
Cedars-Sinai scientists across a variety of disciplines—cardiology, endocrinology, neurology, oncology and more—are dissecting the role inflammation plays in every organ system and disease state. Their research could transform the way COVID-19 is treated—and may open up the possibility that a class of inflammation-thwarting remedies could address nearly every disease.
Inflammation Explained
Our understanding of inflammation dates back to the 1st century, when Roman medical writer Aulus Cornelius Celsus described the four cardinal features of inflammation: heat, swelling, pain and redness. A fifth feature, loss of function, was added later in the century by the Greek medical researcher Galen. Whether you stub your toe, burn a finger or get hit with the coronavirus, your body sends a flood of immune cells to the scene, where they gobble up bacteria, viruses, dead cells and debris.

White blood cells called neutrophils rush to the area to fight infection (they constitute pus). Blood-borne cells called monocytes take up residence inside the tissue. And cells called macrophages (which means “big eaters” in Greek) begin releasing compounds called cytokines, which then sound the alarm for reinforcements. Soon, troops of immune cells flood the site, destroying foreign invaders and damaged tissue in equal measure. Once all of the pathogens are annihilated and the last troops of cytokines attack, the inflammatory process recedes and makes way for healing.
"Inflammation is largely the body's defense mechanism against things that should not be in the body," says Eduardo Marbán, MD, PhD, executive director of the Smidt Heart Institute. "But as with any complicated defense system, any misstep can lead to friendly fire." The same physiological process that reddens the skin around an insect bite and causes swelling in a bum knee can also lead to a host of ailments, ranging from cancer and depression to diabetes and severe cases of COVID-19.
Usually, inflammation enables our bodies to fight off bacteria, viruses and other toxins. But if that immune response continues unchecked, even after the threat has passed, the immune system can turn on healthy tissue. "We have to find a way to target inflammation so that we block its harmful effects without interfering with the beneficial effects," says Prediman K. Shah, MD, director of the Oppenheimer Atherosclerosis Research Center at the Smidt Heart Institute.
In the Blog: Viruses, Bacteria and Fungi: What's the Difference?
It’s that relentless, harmful type of inflammation that’s capturing the attention of scientists and the public. Study protocols and news headlines are increasingly focusing on the deleterious effects of chronic inflammation. It shakes up cholesterol deposits in our arteries, increasing the risk of heart attacks. It gobbles up healthy nerve cells in the brain, leading to memory loss and Alzheimer’s disease. It may even encourage cancerous cells to grow and thrive. Inflammation, as it turns out, could be the engine that drives the most feared diseases, including COVID-19.
Getting to The Heart of Disease
In the 1800s, a German pathologist named Rudolf Virchow suggested that atherosclerosis was an inflammatory disease. “The idea got lost in translation,” Shah says. “That is, until we realized that cholesterol buildup and the subsequent activation of inflammatory cascades within the body are actually what does the most damage to the arteries and organs, whether that’s the heart, the brain or other tissues.”
The immune system views plaque buildup in the arteries as a foreign invader and sends immune cells and other molecules to the scene of the suspected crime. Instead of healing, though, the cells become trapped inside the plaques. It’s likely that chronic inflammation can make these plaques more vulnerable to rupturing.
“We used to think that atherosclerosis was really like buildup of rust in a pipe—a passive process that results from cholesterol deposits in the artery,” Shah says. “Now we know there’s an active component to plaque buildup that involves the immune system and that actually orchestrates the evolution of the plaque, its progression and its eventual destabilization.”
Inflammation can trigger LDL cholesterol (the “bad” type) to latch onto arterial walls, which in turn causes the plaques to become unstable and even burst, leading to clots that cut off the heart’s blood supply. Of course, once a heart attack occurs, inflammatory cells come in to clean up the debris. The body has to strike a perfect balance between clearing up the dead tissue and producing normal, not excessive, healing.

As it turns out, staving off infection could be at the heart of preventing a whole host of diseases.
“People who have gum disease, chronic lung infections and inflammatory diseases, even autoimmune inflammatory diseases, such as rheumatoid arthritis and lupus, are at higher risk of developing heart disease,” says Moshe Arditi, MD, director of the Infectious and Immunologic Disorders Translational Research Center. “Even a mild infection, such as influenza, can make things a lot worse for people who have coronary plaques.”
The reason, he suspects, is that their bodies are already in an inflammatory state. And it may work both ways. An initial infection can set off chronic inflammation that is tied to all sorts of diseases, including inflammatory bowel disease, Alzheimer’s disease and cancer.
Scientists are hard at work trying to devise a way to block the molecules that induce inflammation. The hope, of course, is that one day they’ll be able to prescribe a medication that prevents inflammatory processes from taking a dangerous turn. To some degree, a class of medications called statins already plays that role. “In addition to reducing cholesterol, these drugs also work on reducing inflammation, so it’s a dual pathway,” Arditi says.
Studies show that aspirin, too, not only can protect against heart attacks but also may play a protective role in colon cancer and Alzheimer’s disease by reducing inflammation in the digestive tract and brain. Lifestyle factors, such as diet, exercise and sufficient sleep also keep inflammatory processes in check. So it’s no surprise that these same lifestyle factors can help curb the rate of the nation’s second most common killer: cancer.
Scientists now think that mutation and inflammation are mutually reinforcing processes that can transform normal cells into deadly tumors. “Low-level inflammation feeds cancer cells, encouraging them to grow, thrive and proliferate,” explains Neil Bhowmick, PhD, director of the Cancer Biology Program in the Samuel Oschin Comprehensive Cancer Institute.
Great Communicator
The body’s immune system acts as a gatekeeper, detecting sources of harm and obliterating them before they can do damage. Inflammation is the immune system’s messenger, sharing information between organ systems, including one of the most sensitive and responsive areas: the gut.

"The largest immune network in the body resides in the gut," says Suzanne Devkota, PhD, director of microbiome research in the F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute. As such, the brain and gut send signals back and forth, sounding an alarm when they sense a threat. "It turns out that the gut microbiome—that is, the trillions of microorganisms that live within us and on our skin—profoundly affects both immune responses. We believe it affects brain function, too."
Like security guards at the gates of the digestive system, the immune system’s role is to allow the good guys (like vitamins, minerals, proteins and fatty acids) to enter the body and the bad guys (like toxins and other pathogens) to be turned away.
"Our gastrointestinal tract is essentially a hollow tube from our mouth to our anus, so our bodies are really shaped like a donut," Devkota says. "That means the gut is equally exposed to the outside of our bodies as the inside—and it sees all foreign exposure first. So it makes sense that systemic inflammation likely originates in the gut."
When the gut is operating well, the toxins can’t get past the intestinal cells and their tight junctions. In a healthy digestive tract, the white blood cells never even see the invaders. But if too much bad bacteria infiltrates the gut and the balance of good bacteria to bad is out of whack, the lining of the digestive tract can be damaged—loosening those once-tight junctions.
"But if we take care of our gut by eating a diversity of whole foods, especially fiber-rich fruits and vegetables, and avoiding unnecessary antibiotics, we can potentially delay or stave off systemic inflammation."
With the intestinal barrier that separates microorganisms from the rest of the body is compromised, particles, toxins and bacteria can enter the bloodstream and cause further damage. That breakdown of the gut’s intestinal lining causes the immune system to go into overdrive while trying to take out foreign invaders, which can lead to generalized inflammation that wreaks havoc on every organ system in the body.
"But if we take care of our gut by eating a diversity of whole foods, especially fiber-rich fruits and vegetables, and avoiding unnecessary antibiotics, we can potentially delay or stave off systemic inflammation," Devkota says. In theory, that means we can also make a dent in the incidence of disease states that affect the heart, lungs, joints and brain.
Like the gut, the brain has a gatekeeper to prevent toxins from gaining access to healthy tissue. Called the blood-brain barrier, it acts as a physical barricade while cells called microglia travel through the brain to keep a lookout for possible danger. If the brain is confronted with Parkinson’s disease, Alzheimer’s disease or even an infection like COVID-19 that dumps inflammatory proteins into the blood, the microglia react.
With Alzheimer’s disease, for example, the immune system mistakenly assumes the disease’s plaques and tangles need to be cleared out, so it overreacts, sending in inflammatory cytokines that damage the brain. Unfortunately, healthy brain cells can get caught in friendly fire. Just like the plaques that build up in vessel walls and begin churning out inflammatory proteins, the influx of toxic proteins in the brain transforms protective microglia into disease-like cells.
"Instead of protecting healthy brain cells, these disease-associated microglia begin pumping out high levels of inflammatory proteins that exacerbate neurodegenerative processes," says Maya Koronyo, PhD, an Alzheimer’s disease and neuroimmunology research scientist. "That’s why tackling neuroinflammation early in the disease process is key to fighting the disease."
The idea is to return diseased-associated microglia to their protective state. Then those healthy microglia can communicate with other cells in the body that the threat has passed, ultimately restoring blood flow to once-diseased vessels, in a sort of positive snowball effect.
"What we need is a multi-targeted approach to strengthen the types of cells that are protective and dump some cells that could be overly reactive," Koronyo says.
Counteracting Inflammaging
The Inflammatory Process
Chronic inflammation triggers a cascade of effects in the body. Here’s a rough sketch of how it works:
- Something triggers the immune system. Whether a paper cut, chronic disease or novel coronavirus, your body goes on the defensive.
- The immune system launches an attack. The body responds with an inflammatory process, including blood vessel expansion, to increase blood flow to affected areas.
- Instead of receding when the threat is gone, the immune system continues to attack.
- Inflammatory chemicals continue to flood the area, damaging healthy tissue. Over time, this chronic, low-grade inflammation can lead to diseases like cancer, heart disease, dementia, arthritis and depression.
There's no doubt that inflammation plays a critical role in health and wellbeing. We need it to protect against infection, heal a broken bone or skinned knee, and even to clear out the muck in our brains so we're able to think straight. Unfortunately, the aging immune system may struggle with mounting the response needed to attack invading pathogens while limiting the collateral damage.
"With aging, our bodies undergo a process called immunosenescence, or aging of the immune system," Koronyo says. "So it's not only your brain and heart that are aging, and your skin that is wrinkling, but there's also a specific process that causes the immune cells to become less responsive and ultimately ineffective."
The same immune cells that mount a response against a pathogen are at work with aging. But instead of an acute, high-level response, it's a sort of low-grade, unresolved inflammation that hums in the background. This type of inflammation is called "inflammaging."
"Inflammaging is a sort of chronic, nagging inflammatory response that doesn't fight anything. Instead, it builds up over time, damaging tissues," says immunologist Goodridge. The age-old question, of course, is how to turn down that response without compromising the body's defense against pathogens.
Unfortunately, doctors can't fight inflammation effectively with current anti-inflammatory medications. They inhibit the body's ability to fight infection and they can also worsen the disease states that doctors are trying to overcome. Ibuprofen, for example, can cause stomach bleeding and increase blood pressure. There's even emerging evidence that heavy use of NSAIDs, like ibuprofen and aspirin, might speed up the progression of Alzheimer's disease among patients in the most advanced stages.
The ideal solution would dampen the damaging impact of inflammation without diminishing its healing effects. To that end, Cedars-Sinai scientists are hard at work identifying agents that specifically target the harmful portions of the inflammatory response and shut it down before it spins out of control.
In the not-too-distant future, doctors may even be able to help their patients turn back the clock on inflammaging. Cedars-Sinai researchers are studying anti-aging factors in the blood.
"We did a study where we transplanted bone marrow from young mice into old mice, like a bone marrow transplant," Goodridge says. "Six months later, the old mice had improved learning and memory, and less inflammation in their brains." She notes that investigators are still trying to determine if it's more important to reduce pro-aging factors or replace anti-aging factors—or do both.
While those treatments are still years down the road, you can do plenty of things to help lower your inflammatory load in the meantime. "It's highly likely that living a lifestyle that limits systemic inflammation and infection is going to diminish the negative effects of aging," Koronyo says. "Ample evidence shows that leading a healthy lifestyle decreases your risk of chronic diseases."
The basic tenets of that healthy lifestyle probably sound familiar: Exercise, eat a whole-food, plant-based diet that limits sugar and saturated fat, and practice stress-reduction strategies, such as meditation, yoga and deep breathing. Most important, get your annual flu shot (data show that getting vaccinated against the flu significantly reduces the risk of heart attacks and even Alzheimer's disease) and get plenty of sleep. Your body will thank you.
Model of Inflammation
Although inflammation is a hallmark of COVID-19, the triggering mechanisms remained a question mark. Consequently, Moshe Arditi, MD, director of the Cedars-Sinai Pediatric Infectious Diseases and Immunology Division, worked with a colleague to zero in on a protein of SARS-CoV-2 (the novel coronavirus), called superantigen, that can kick the immune system into a dangerous overdrive akin to toxic shock syndrome.
The team used a computer model to detail the interaction between the SARS-CoV-2 protein and T cells. As soldiers of the immune system, T cells fight off infections. But when too many are enlisted, they generate massive amounts of inflammatory cytokines—proteins crucial to immune-system signaling—in what’s called a “cytokine storm.”
Arditi was drawn to the mystery after seeing early reports of a condition called multisystem inflammatory syndrome in children (MIS-C) that had been identified in pediatric COVID-19 patients. The syndrome is rare—which is fortunate, as it can be fatal.
Discovering the protein-level similarities between SARS-CoV-2 and the bacterial structure that causes toxic shock syndrome could lead to better treatments—not only for MIS-C patients, but also for adults with COVID-19 who experience a cytokine storm.