Routine Liver Biopsies During Bariatric Surgery Help Catch NAFLD Early
Date
January 24, 2022
Date
January 24, 2022
Credits
Medical providers featured in this article

In Brief
{{cta-block}}
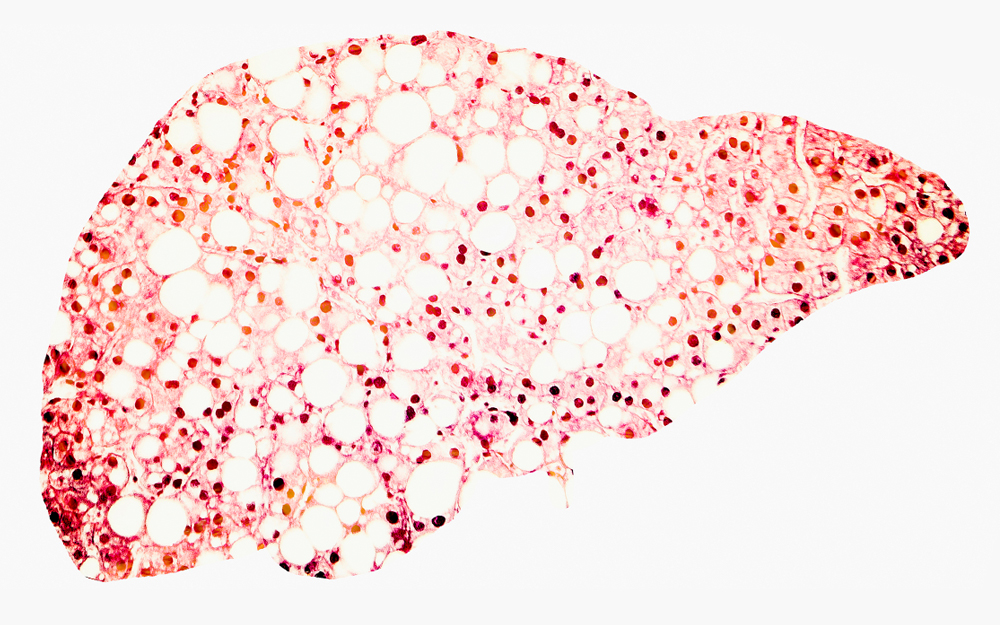
Nonalcoholic steatohepatitis (NASH), an advanced form of nonalcoholic fatty liver disease (NAFLD), is caused by a buildup of fat in the liver and common in patients with obesity. According to the National Institute of Diabetes and Digestive and Kidney Diseases, research suggests NAFLD "is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity."
"This research reinforces that weight loss surgery is not just about losing weight. It’s also about improving overall health. With this research in mind, we can think about the purpose of bariatric surgery as both helping the patient lose weight and identifying other related problems that can impact their long-term health."
"NASH can lead to scarring of the liver—or cirrhosis—which can be a very serious condition," says Miguel Burch, MD, chief of Minimally Invasive and GI Surgery at Cedars-Sinai. "With obesity becoming more and more prevalent around the world, cirrhosis associated with fatty liver disease may become one of our biggest health issues as a society."
NASH is diagnosed through liver biopsy. Some, but not all, surgeons include routine liver biopsies when performing bariatric surgery, given the high prevalence of NASH in overweight patients. Cedars-Sinai researchers took a closer look at this practice to help determine the risks and benefits of routine liver biopsy during bariatric surgery.
Rating the risk of liver biopsy
The study began with a retrospective analysis of Cedars-Sinai data regarding patients who underwent bariatric surgery with concurrent livery biopsy between 2016 and 2020. The team compared patients who received liver biopsy and those who did not, and included demographics and postoperative outcomes.
"We took a look at potential complications that could arise due to liver biopsy and we did not find any difference between the group that received liver biopsy as part of bariatric surgery and the group that did not," says Mazen Noureddin, MD, director of the Fatty Liver Program at Cedars-Sinai and coauthor of the study.
Specifically, the study found no differences in postoperative complications, blood transfusions, readmissions or reoperations when comparing the two groups.
The ultimate conclusion is that routine liver biopsies during bariatric surgery identify higher rates of advanced NAFLD compared to selective biopsies and can be performed safely without increased risk to patients.
"We found that routine liver biopsy can identify patients whose livers might look reasonably normal at first but actually have more advanced disease than we would have thought," said Burch.
Benefits beyond weight loss
The benefit of routine liver biopsy during bariatric surgery is the identification of potential conditions early in their progression.
"When looking at the patient data, we found a significant number of patients impacted by fatty liver disease, inflammation and fibrosis," says Noureddin. "It’s important for us to be able to address these concerns to ensure the patient is not at high risk for something like liver cancer."
The team hopes these findings will encourage physicians to consider the extra step of liver biopsy during bariatric surgery to get a full picture of the patient’s health and, in turn, improve their overall quality of care.
"This research reinforces that weight loss surgery is not just about losing weight," says Burch. "It’s also about improving overall health. With this research in mind, we can think about the purpose of bariatric surgery as both helping the patient lose weight and identifying other related problems that can impact their long-term health."