The Rise of the Organoids
Date
December 22, 2025

Date
December 22, 2025
Medical providers featured in this article

In Brief
- The Cedars-Sinai Board of Governors Regenerative Medicine Institute is uniquely positioned to help researchers work with iPSCs and organoids, which provide human-based research models that are personalized to patients and/or diseases.
- Cedars-Sinai research is leveraging brain organoids to investigate pediatric tumorigenesis and treatments.
- Investigators are also launching iPSCs into space, hoping to create heart and brain organoids in microgravity.
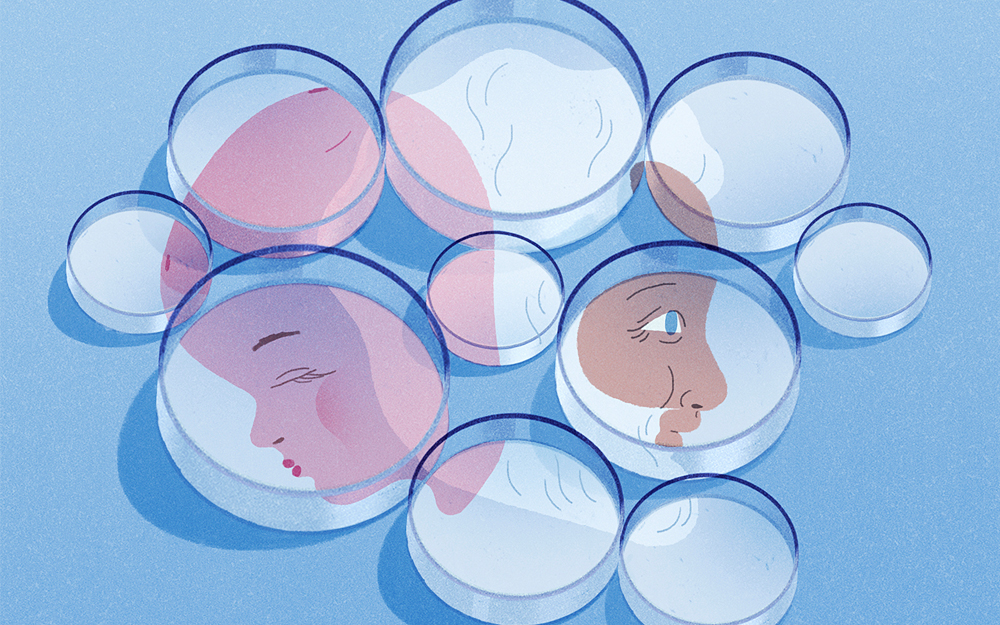
Organoids are at the leading edge of new biomedical research.
These 3D human-based models that mimic real organs can easily be generated at scale for drug testing and disease modeling and can be personalized to specific patients. Cedars-Sinai investigators are leveraging them to tackle a multitude of diseases.
Joshua Breunig, PhD, research scientist and director of the Cell, Organoid and Cancer Engineering Special Resource at the Cedars-Sinai Board of Governors Regenerative Medicine Institute, is investigating a pediatric glioma using organoid models of the disease. The treatment protocol he and his team have discovered will soon enter clinical trials.
“We’re hoping these organoids will be predictive and save kids’ lives,” he said.
Over the past 15 years, the institute has pioneered the development of induced pluripotent stem cell (iPSC)-based organoids. It manages extensive tissue banks representing a broad cross section of diseases and runs a shared resource laboratory with the most up-to-date technology, training and resources for interested investigators.
“You can make organoids of any organ and disease you want, from a patient’s own cells, and you can make as many as you need,” said Clive Svendsen, PhD, executive director of the Regenerative Medicine Institute. “It’s so much more efficient for drug trials and disease modeling. That’s why there’s such excitement around this technology.”
A Valuable Research Tool
With the National Institutes of Health’s (NIH) recent initiative to “prioritize human-based research technologies,” organoids and related models present an exciting and viable solution—one Cedars-Sinai is strategically positioned to exploit.
At the Regenerative Medicine Institute, organoids are grown using iPSCs—adult somatic cells that have been brought back to a stem cell state and can be guided to form any cell type in the body. But while iPSCs lie flat in a dish, organoids develop into tiny 3D structures that include many of the cells present in whichever human organ is being grown. Brain, heart, kidney, liver, lung, pancreas—any organ can be represented in organoid form.
Human-based organoids provide many clear advantages over nonhuman models.
“The human brain develops very differently from that of a fly, bird or mouse,” said Breunig who is the Ben Winters Chair in Regenerative Medicine at Cedars-Sinai. “And it’s not just the brain; many important biological characteristics aren’t conserved between mice and humans.”
Organoid models are also efficient and accurate precursors for clinical trials.
“If a drug only works in 10% of the test subjects, it’s a failure,” said Svendsen, who is the Kerry and Simone Vickar Family Foundation Distinguished Chair in Regenerative Medicine at Cedars-Sinai. “But if you can use organoids ahead of time to identify the 10% that will be helped by the drug, you can limit your trial to those patients. Now you’ve got a solution that provides a more direct path to success.”
Organoids in Action
Breunig’s laboratory is growing brain organoids to investigate pediatric tumorigenesis and treatments.
“With organoids, we can make better in vitro models that recapitulate each individual patient’s tumor in a primary human system,” said Breunig.
The laboratory makes brain organoids from iPSCs, which grow to include many of the cells and some of the structures seen in a developing human brain. A small subset of cells is mutated with the exact mutations derived from a given patient. In time, the tumor grows to take over the entire organoid and becomes a self-renewing 3D brain tumor model.
“Brain tumors, particularly pediatric brain tumors, are rare,” said Breunig. “You could never find enough human patients to participate in all these clinical trials; but with organoids, we can do it relatively easily in a dish.”
Breunig’s laboratory is bombarding the cancerous brain organoids with radiation, chemotherapy and any number of other multidimensional therapeutics to discover the most effective approaches to treatment.
Using this method, the laboratory uncovered a metabolic vulnerability in a subtype of pediatric gliomas that makes up 50% of these cancers in young patients. The team has identified an agent that effectively exploits the vulnerability. An upcoming clinical trial—in partnership with Children’s Hospital Los Angeles and the Pediatric Neuro Oncology Consortium—will test the therapy.
The organoids could be lifesaving and could save young patients’ time by making sure they get the most effective treatment, Breunig said.
Additionally, Arun Sharma, PhD, a research scientist at the Regenerative Medicine Institute and the Smidt Heart Institute at Cedars-Sinai, is leveraging heart organoids and spheroids—a simpler tissue cluster—to test the toxicity of the cancer drug doxorubicin.
“This cancer drug causes heart failure in a small number of patients; however, it is unclear which patients are susceptible,” Sharma explained. “Using patient-derived heart organoids and spheroids, we can potentially screen people and clear them to use the drug.”
A safer version of doxorubicin that Sharma’s laboratory helped validate is now being moved toward clinical trials.

Pushing the Limits
Regenerative Medicine Institute investigators are addressing obstacles that limit organoids’ ability to replicate human biology. The models cannot mimic a complete, holistic body to predict how the immune system, for example, might respond to treatments. And since they lack circulatory systems, they’re limited to a microscopic size because without perfusion, the central cells become necrotic from lack of sustenance as the organoid grows. Also, organoids represent organs in an immature state, so results may not translate as effectively to adult conditions.
Breunig’s laboratory is attempting to seed organoids with missing cells so they better resemble the bodily environment.
“We’re hoping to use transcription factors to specify cell types we might be missing,” Breunig said. “Just sprinkle some programmed cells into the organoid that we can induce later to make cells like microglia or endothelial cells that otherwise do not appear in the organoids.”
Another approach under consideration is to connect organoids to other vascularized human models, such as organs-on-a-chip.
The Promise of Space
Other solutions to shortcomings in organoid technology may be found in an unlikely place: outer space.
Cedars-Sinai recently launched its sixth mission to the International Space Station with iPSCs. The plan is to use these stem cells to create heart and brain organoids in space for the first time.
“The value of doing this in microgravity is that the stem cells can naturally float and develop into 3D systems,” said Sharma, who also directs the Cedars-Sinai Center for Space Medicine Research. “Organoids should grow better in space than they do on Earth, where they are flattened by gravity.”
Growing the organoids in microgravity might even allow for the development of blood vessels and other cell structures that have so far largely eluded researchers growing organoids on Earth, Sharma said.
In addition, human cells and organs appear to age much faster in microgravity—a process linked to a lack of biomechanical pull on the cells’ interior and the possible effects of space irradiation. This effect plays havoc with the bodies of astronauts on the space station, who are forced to exercise for two to three hours a day to combat the rapid degradation of their muscles and bones.
But if the space environment can accelerate the aging of organoids, it may be a boon for investigations of the diseases of aging, such as heart disease, Alzheimer’s disease and amyotrophic lateral sclerosis (ALS). Svendsen and Sharma see a future in which automated drug screening on these organoids can be performed aboard orbiting satellites and results reported down to doctors and researchers on Earth.
Needed: New Models
The NIH announced in April that it plans to prioritize “cutting-edge alternative nonanimal research models,” expanding funding for human-based research approaches and limiting funding for those that are solely animal-based.
Svendsen would prefer scientists be given the freedom to use the models that best suit their research. Still, as a pioneer in stem cell technologies, human models of disease and iPSC-derived organoids, the Regenerative Medicine Institute is uniquely positioned to help biomedical researchers incorporate the most advanced nonanimal technology into their work, he said.
“We’ve been developing this technology for 15 years,” said Sharma. “We have large stocks of stem cells for Alzheimer’s, ALS, heart disease, liver and kidney disease, and cancers, and we can turn those into models of human organs.”
The institute has also invested significant resources in the most up-to-date technical equipment for the manufacture and analysis of stem cells and organoids, including the building of the Cedars-Sinai Biomanufacturing Center. Stem cell and organoid technology can be expensive, but the center has the capacity to produce large quantities of stem cells and organoids, taking advantage of economies of scale.
“We’re better prepared than just about any other institution in the U.S. for this moment,” said Svendsen.
The Shared Resource Laboratory
In 2024, the California Institute for Regenerative Medicine (CIRM) awarded the Regenerative Medicine Institute a $4 million infrastructure grant to create a new shared resource laboratory. One of 11 such laboratories in California, the Organoid and Organ-Chip Shared Resources Laboratory at Cedars-Sinai is available to share its expertise and technology with biomedical researchers across California.
“We have so much experience here, and we’re now providing training and resources for researchers who want to learn how to do this work with iPSCs and organoids,” Sharma said.