How Virtual Brain Tumors Are Transforming Cancer Care
Date
December 29, 2025
Date
December 29, 2025
Medical providers featured in this article
In Brief
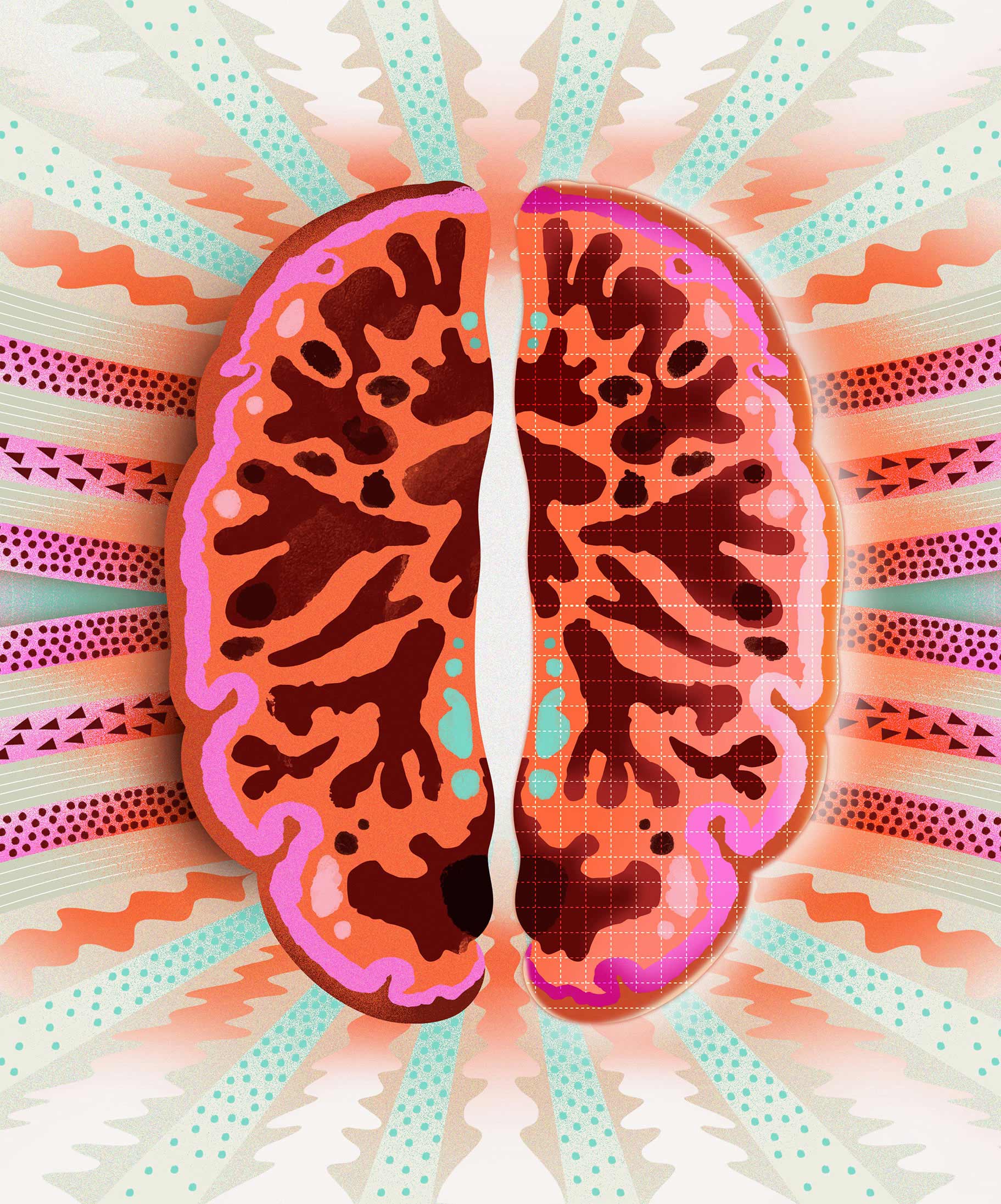
- Using predictive modeling, Cedars-Sinai researchers can determine how brain tumors grow, spread and respond to therapy.
- Kristin Swanson, PhD—a world leader in the new field of mathematical neuro-oncology—is bringing precision models to patient care.
- Mathematical neuro-oncology integrates physics, imaging, AI and biology to create computational forecasts of each patient’s unique tumor.
- Swanson’s models offer a powerful tool for patient selection, helping clinical trial sponsors enroll participants whose tumors are predicted to be biologically vulnerable to the drug being tested.
Brain tumors present among the most formidable challenges in medicine. Glioblastoma—the most common malignant brain tumor in adults—has a median survival of less than 15 months, even after treatment with surgery, radiation and chemotherapy. Unfortunately, even resection of the entire visible mass is often incomplete, resulting in remnants of microscopic cancer tendrils that often infiltrate surrounding tissue. Recurrence is essentially inevitable.
But what if doctors could see beyond the visible cancer mass on scans? What if they could not only determine where the tumor is, but predict where it is spreading—and which tools can best target the tumor cells?
“In many ways, my work is like weather forecasting for brain cancer,” said Kristin Swanson, PhD, a pioneer in the field of mathematical neuro-oncology and Cedars-Sinai faculty member with joint appointments in the Department of Neurosurgery, the Department of Computational Biomedicine, and the Department of Pathology and Laboratory Medicine. “Just like how meteorologists use satellite images to predict when and where a storm will hit, we use patients’ MRIs and physics to model how tumor cells move through each patient’s brain.”
Using advanced modeling technology that hinges on physics, Swanson’s team creates virtual versions of a patient’s tumor to simulate how it grows, spreads and responds to therapy. Their goal is to bring a level of predictive modeling to a seemingly unpredictable disease process.
An Inspiring Origin Story
Swanson’s professional roots in both mathematics and medicine led her organically to mathematical oncology. Her passion for the work is not purely academic, but also personal. Swanson’s father, who inspired her love of numbers with algebra puzzles at the kitchen table, died of lung cancer during her senior year of college.
“Watching him go through treatment, I saw how much cancer care relied on averages, not on the individual patient,” she said. “Even then, I knew that wasn’t good enough.”
Swanson set out to bring quantitative precision to cancer care, pursuing a PhD in applied mathematics and studying under J. D. Murray, PhD, a world leader in mathematical biology. At the time, in the mid-1990s, very few scientists were working at the intersection of mathematics and medicine in ways that could impact patient care.
“I was heckled off stage more than once,” Swanson said about her early lectures in this space. “People told me that if I was so good at predicting things, I should go to Wall Street.”
Instead, Swanson stayed the course and helped define a new scientific field: mathematical neuro-oncology. Her approach integrates physics, imaging, AI and biology to create computational models of each patient’s unique tumor—a so-called “digital twin.”

The Power and Possibility of Digital Models
Swanson’s virtual replicas integrate multiple layers of patient data into a single predictive framework. By calibrating models with both imaging and biopsy information, Swanson’s team can uncover tumor cells that evade detection on MRI and map their likely trajectories through normal-appearing brain tissue.
One model predicts how a tumor will grow and spread. Another, trained on massive datasets of image-localized biopsies, translates subtle MRI features into biological signatures such as cell density, proliferation rates and immune activity.
In many ways, my work is like weather forecasting for brain cancer. Just like how meteorologists use satellite images to predict when and where a storm will hit, we use patients’ MRIs and physics to model how tumor cells move through each patient’s brain.
Together, these models simulate how a tumor will evolve and how it might respond to specific therapies.
“The models don’t just look like the individual patient’s tumor; they behave like it, too,” Swanson said. “That allows us to try different treatment strategies virtually before we commit to a plan in real life. Moreover, each time we obtain a new MRI scan for a given patient, we can update our digital twin model to further hone our predictions for that patient.”
These image-based tools hold tremendous potential in the context of immunotherapy, where patients’ responses are highly variable and hard to measure with standard imaging technology. For example, by detecting subtle shifts in T-cell activity, the tools can determine whether the immune system is responding to the tumor—even when evidence from MRIs alone is inconclusive.
“Interpreting an MRI after immunotherapy is very difficult, as the immune response associated with tumor regression mimics that of tumor growth,” said Swanson. “Our models help clarify that picture, and when we see the right kind of signal, we can say with confidence that the therapy is working.”
From Clinical Trials to Clinical Tools
The digital twins are already showing promise in early-phase research, not only in tracking treatment response but in pairing patients with the right clinical trials. Patient selection is critical in glioblastoma because tumors are highly heterogenous and tissue access is limited.
“Clinical trials typically treat every patient and every tumor the same,” Swanson said. “But if we can use imaging and modeling to identify the patients most likely to benefit from a specific therapy, we can improve trial outcomes, reduce time to approval and spare patients from ineffective therapies.”
With nearly $14 million in grant support from the National Cancer Institute, Swanson’s laboratory is scaling this work across brain tumor types and working toward U.S. Food and Drug Administration approval so digital twins can be formally integrated into trial design and, eventually, clinical care.
At Cedars-Sinai, Swanson has found the ideal environment for that vision.
“Very few institutions bring together neuro-oncology, advanced imaging, computational medicine and the highest-quality clinical care all under one roof,” she said.
Swanson’s approach could mark a turning point in brain cancer care. Her models expose the hidden complexities of each tumor, charting a course toward more effective, individualized treatment strategies.
“Every patient deserves their own equation,” said Swanson. “Instead of relying on averages, we can finally tailor treatment to the unique biology of each tumor.”