The History of Medicine Can Inform the Future
Date
October 21, 2022
Credits
Date
October 21, 2022
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Even if the letters "PhD" or "MD" follow your name, your training in science or medicine may not be complete. Not only is the history of medicine fascinating in its own right, it can uproot assumptions, disrupt bias and point the way to a better future, says medical historian Gideon Manning, PhD.
"Cedars-Sinai houses the only substantive history of medicine program embedded within an independent academic medical center," says Dr. Manning, director of the History of Medicine Program in the Department of Biomedical Sciences. "We are a research group that in a few short years has become a scholarly destination welcoming speakers and researchers from around the world."
History of medicine is one of many areas in the humanities and the arts that promotes the well-being of someone at work, but also more generally."
– Gideon Manning, PhD
The program was recently accepted into the Consortium for History of Science, Technology and Medicine, a Philadelphia-based organization that brings together a select group of educational, cultural and scientific institutions to promote public understanding of the history of science, technology and medicine. Inclusion is a rare honor and Cedars-Sinai is the only academic hospital to be a member institution.
The History of Medicine Program offers a biweekly speakers’ series that hosts notable historians of medicine and science along with six-week courses focused on topics as varied as the Jewish medical tradition, the history of pathology and the history of women in medicine. Cedars-Sinai also recently launched the Center for Medicine, Holocaust and Genocide Studies under the auspices of the History of Medicine Program.
"Part of what’s unique about the way we do history of medicine here at Cedars-Sinai is that we are constantly rubbing shoulders with our colleagues on the clinical and research sides to the benefit of all of us," Dr. Manning says.
Why should clinicians or scientists invest in learning about the history of medicine?
Gideon Manning: It’s a good question. But the question assumes something my own experience makes me want to resist. It assumes the practice of medicine is somehow distinct from the history of the field and one’s identity as a physician or professional. Those identities are not static; they have a history, and to assume them in the present is to implicitly endorse their history.
The question also unnecessarily separates the practice of medicine from broader quality of life questions. There’s now an important movement in medical education to recognize real phenomena like burnout and the long-term well-being of medical providers.
The history of medicine is unique among the humanities and the arts in that it simultaneously promotes a deeper understanding of one’s professional identity while also enriching one’s life more generally. It is the history of something uniquely human, namely our struggle to understand and maintain what it is to live a healthy life and have a comfortable death.
So the history of medicine shouldn’t be considered a separate topic from medicine itself?
GM: Medicine has long been called an art and a science, though what that means precisely has changed over time. In the last few decades, the emphasis has been so heavily on the science, however, that something of the art has arguably been lost.
The history of medicine can remind us of the ways in which the science and the art of medicine have evolved and the ways in which both have always been relevant. We can see moments in the past where one or the other haven’t been respected to the detriment of patients and society.
For example, take the current COVID-19 pandemic. Knowledge of the history of epidemics and pandemics, if it was more on the surface of people’s awareness, would have allowed us to anticipate some of what was going to happen and avoid some of the social marketing missteps related to vaccines.
There were also economic lessons to be taken, as well as awareness of the intersection of health and ethnicity in the presence of new pathogens. Pursuing medicine without the history of medicine raises the risk of blinding us to things we ought to know and are best not relearned the hard way.
How can we make sure we don’t lose the lessons we are learning from this pandemic?
GM: We have established a COVID-19 archive to document how our hospital has responded to and been affected by the pandemic. It includes oral histories and a document archive comprising interviews with physicians and staff, describing what their life at the hospital was like before and how it changed.
This will be a scholarly repository for people around the world and an opportunity for Cedars-Sinai to memorialize the efforts of so many, including what worked and how the pandemic was accommodated. Right now we are all pandemic historians, still living this experience, but many of us are trying to move on and over time we will forget. The historians of medicine are making sure the knowledge is not lost.
Outside of the pandemic, how else can our knowledge of history improve our understanding of medicine today?
GM: There are a lot of things we take for granted concerning the organization of medical knowledge, who should be a physician and who qualifies as being ill. These assumptions have histories and when you look carefully at the emergence of a scientific medical culture, you see it is a human creation that took shape over a long period of time.
Let me offer an analogy. Medicine is like a building that has taken generations to complete though it’s never really done. If you look carefully at such a building, with the right training, you will find evidence of builders’ hesitation or incompetence, and you’ll likely notice some of the parts don’t quite fit together for the simple reason that there were different builders over time with different priorities and interests.
All to say, studying the history of the building can help us understand and explain why the building looks as it does and why the floors creak and the ceiling leaks. In medicine, history can illuminate why some things don’t work so well today and what might be changed in the future because it needn’t be the way it is.
Can you provide an example of how 'builders'' assumptions and interests have influenced the course of medicine in an unfortunate way?
GM: Take the case of sickle cell anemia: we knew all the genetic information we needed to know about the disease even before the human genome project was complete. But research into the condition wasn’t pursued because it predominantly affects people of recent African descent, and they haven’t had a sizable voice in medical research. We need more diversity and inclusion in medical research to fix the problem.
There are long-standing disparities in heart health between men and women. Assumptions about whose voice matters, who gets sick with what disease, or simply who can be a scientist or a physician are at the root of many of these disparities. The history of medicine is, in part, about bringing attention to the contexts in which these assumptions have taken hold, and in so doing directing us to those places where the floors creak and the roof leaks in modern medicine. Historians of medicine, like the rest of us, are out to fix these disparities, we just carry slightly different tools in our toolbox.
What is your research focus?
GM: I study primarily 15th-18th century medicine, which represents a pivotal moment in the development of our scientific medical culture. At the beginning of the period I study there was no scientific medicine, at least not in our sense, but at the end of the period there surely was.
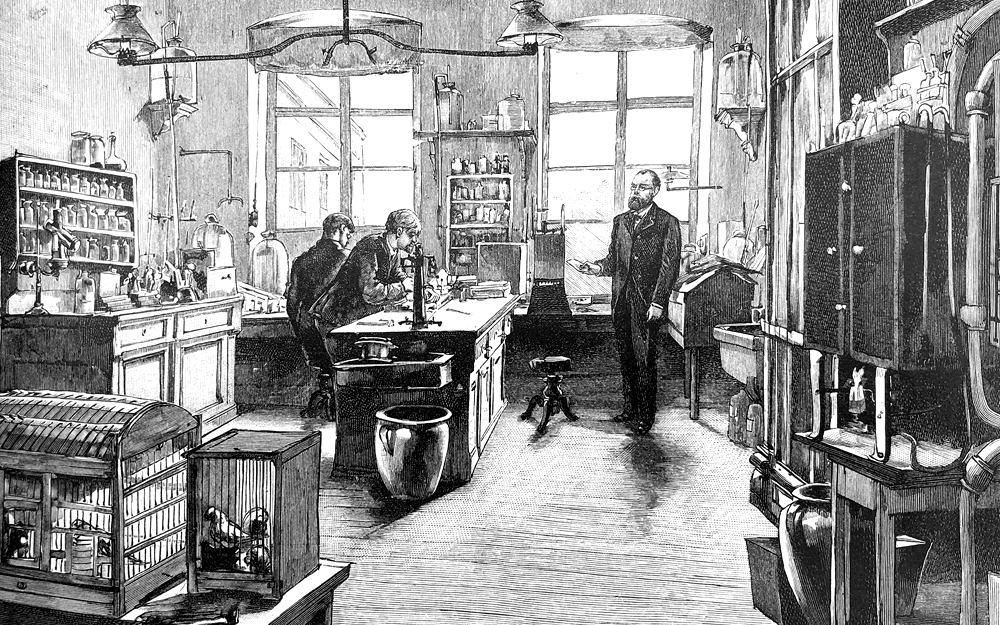
It was a time of scientific revolutions: the establishment of colleges and medical societies, the appearance of journal publications and books with images of anatomy, the rise of quantification and data analysis. Those advances created our world: journals became the standard for how scientific knowledge is shared, with short readable peer-reviewed research becoming the norm.
The laboratory shaped how science is conducted, with divisions of labor within a hierarchical and specially trained group, creating a perceived separation between scientists, clinicians and the public at large. Counting things became the way data is understood, with consequences still being felt in clinical studies and computational medicine.
Is there a revelation you’ve experienced as a historian of medicine that you would like to share with others?
GM: One of the projects I’m involved in is a book about the history of death in a broad sense. During a research year in medical school, I came to believe that death is best seen as a historical event in the fullest sense of that term. It’s a biological event, it’s a medical event, it’s an economic event, it’s a cultural event, it’s an artistic event, it’s a social event. It’s even a political event—think of the way governments use the moment of death to change laws and exercise power.
All this is easiest to see when death happens on a massive scale, as during wars or pandemics, but it’s also true on an individual level. I’m exploring what it is to understand death in this broad sense, and how knowledge from all sides could influence patients and doctors alike to have conversations at the end of life.
Who’s teaching in the History of Medicine Program?
The History of Medicine Program offers instruction from a group of faculty members with widely varied training and expertise.
"One of the great strengths of our program is we were each trained at different institutions and have a range of interests," Dr. Manning says.
Meet the team:
Leon Fine, MD
Research focus: Arts and humanities in medicine.
Latest passion: Origins of gastronomy and food culture in France.
Favorite rare book: Out of the many rare books in his collection, Dr. Fine is particularly fond of Jean-Anthelme Brillat-Savarin’s La Physiologie du Gout (The Physiology of Taste), 1826. This first edition is in its original state.
Kirsten Moore-Sheeley, PhD
Research focus: History of disease control, biomedical science and technology, and global health.
Work in progress: Project about the history of failed and difficult-to-produce vaccines.
Productivity playlist: Dr. Moore-Sheeley vibes out to Marcus Miller and other jazz bassists while she works.
Rena Selya, PhD, MLIS
Research focus: 20th-century American biomedicine, focusing on the history of genetics, molecular biology, cancer research and neuroscience.
Work in progress: Book on Salvador Luria, an Italian Jewish refugee microbiologist who won the 1969 Nobel Prize in Physiology or Medicine for “discoveries concerning the replication mechanism and the genetic structure of viruses.” He was a passionate political activist throughout his life in the United States.
Cool climber: Dr. Selya recently hiked Exit Glacier in Alaska.
Sari J. Siegel, PhD
Founding director of the Center for Medicine, Holocaust and Genocide Studies
Research focus: Medicine and the Holocaust.
Work in progress: Book on Jewish prisoner-physicians in Nazi camps; contributor to the Lancet Commission on Medicine and the Holocaust: Historical Evidence, Implications for Today, Teaching for Tomorrow
Past passion: Dr. Siegel is a former medical student with a passion for sports medicine.
Gideon Manning, PhD
Research focus: Changing conceptions of human and animal bodies, life, death, health, and nature—along with the emergence of our scientific medical culture.
Work in progress: Papers discussing the history of anatomical illustration, evolving conceptions of surgical success, early bio-mechanical theories in physiology, and a book on the many perspectives from which people experience and understand death.
PhD of pie: During the initial two years of the pandemic, Dr. Manning learned to bake nearly 50 different pie recipes.





