Understanding Vascular Malformations
Date
December 16, 2022

Date
December 16, 2022
Credits
Medical providers featured in this article

In Brief
{{cta-block}}
A vast network of blood vessels feeds the brain needed oxygen and nutrients, but sometimes, that structure gets compromised. Vascular malformations can be congenital or develop or worsen after an accident or blood clot.
"Vascular malformations can affect patients of all ages," says Cedars-Sinai vascular neurosurgeon Dr. Nestor Gonzalez.
{{providers}}
These lesions affect around 1% of Americans, according to the National Institutes of Health. While most malformations can be safely left under observation, others can trigger serious, life-threatening complications in the blood vessels, brain and spinal cord. It's critical for your doctor to determine what's happening at the vascular level. They should carefully consider your risks and work closely with you on a treatment plan, Dr. Gonzalez stresses.
"When someone is diagnosed with a vascular malformation, there is a natural fear," he says. "It's the sensation that we have a ticking time bomb in the head that can explode at any moment."
"That fear is normal—and needs to be addressed," he cautions.
"People of all ages can have a vascular malformation."
Vascular malformation types
In healthy vascular systems, arteries are routed like a large tree trunk through the neck, breaking up in the brain into narrowing branches of tiny vessels known as capillaries. These capillaries pool into veins that then become larger, Dr. Gonzalez explains.
When those connections are abnormally built or disrupted, pressure can build and cause bleedings, swelling or seizures.
Vascular abnormalities include:
- Arteriovenous malformations (AVMs)
- Arteriovenous fistulas (AVFs)
- Cavernous angiomas (cavernomas)
- Capillary telangiectasias
- Developmental venous anomalies (DVAs)
- Capillary malformation-arteriovenous malformation syndrome (CM-AVM)
- Hereditary hemorrhagic telangiectasias
AVMs—tangled knots of blood vessels—can form instead of capillaries. Usually present at birth, they're among the most common vascular lesions, affecting about 30,000 Americans, according to the National Organization for Rare Disorders.
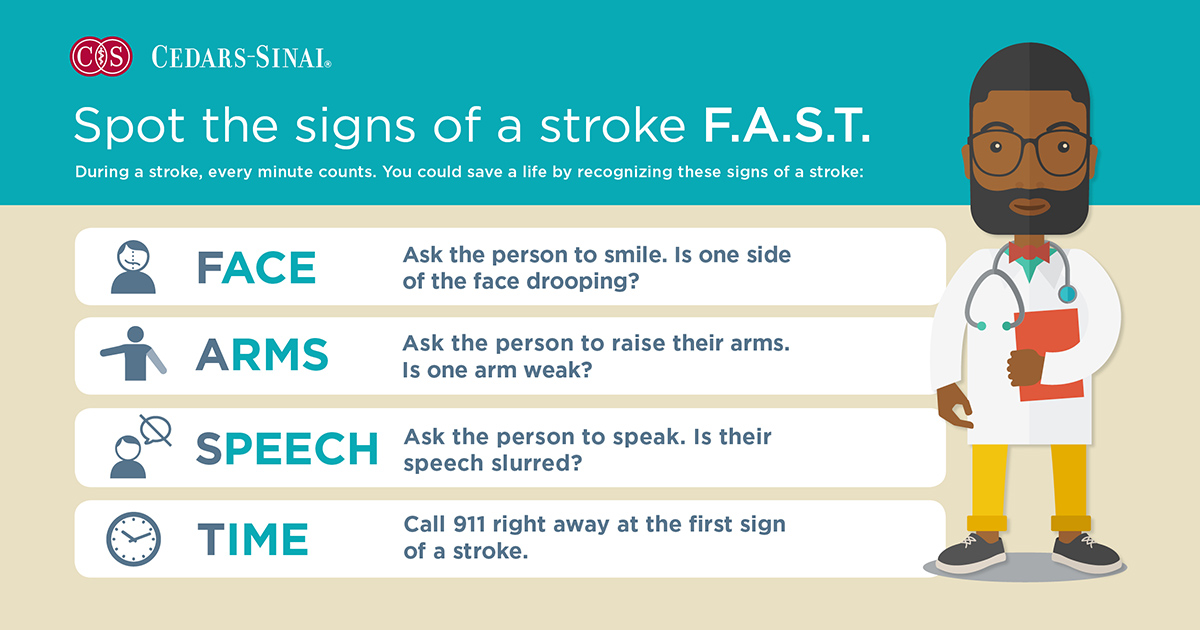
People with an AVM might experience headaches, vision, speech, and movement changes, dizziness or seizures.
These lesions interrupt the artery-vein link and normal bloodflow to brain tissue. As vessels expand and wear out, they can burst and cause bleeding, the American Stroke Association notes. Uncontrolled brain hemorrhage can cause stroke, brain damage or even death.
Fistulas disrupt the vascular network as well, connecting arteries to veins directly. Pressure goes up, and veins can clog, triggering similar neurological symptoms. AVFs can happen in either the brain or spinal cord after an injury or accident, Dr. Gonzalez cautions.
Cavernomas, which often run in families, are congenital "berry-like" blood vessel masses. These lesions are lower pressure but chronic, leaking small traces of blood over time and irritating the brain. Seizures are a common manifestation.
Usually asymptomatic, capillary telangiectasias (dilated capillaries) and developmental venous anomalies (when veins drain blood differently, through a splintered, palm-tree-like structure) are the most harmless.
Some genetic conditions, such as CM-AVM syndrome and hereditary hemorrhagic telangiectasia, lead to a combination of multiple blood vessel malformations. Patients often have strong family histories, skin markings and systemic health problems of nosebleeds, headaches, fistulas, brain bleeds and lung abnormalities.
Diagnosing vascular malformations
Some vascular changes are visible, like the prominent port-wine stain birthmarks in CM-AVM.
Many, though, can't be seen by the naked eye and cause little to no symptoms.
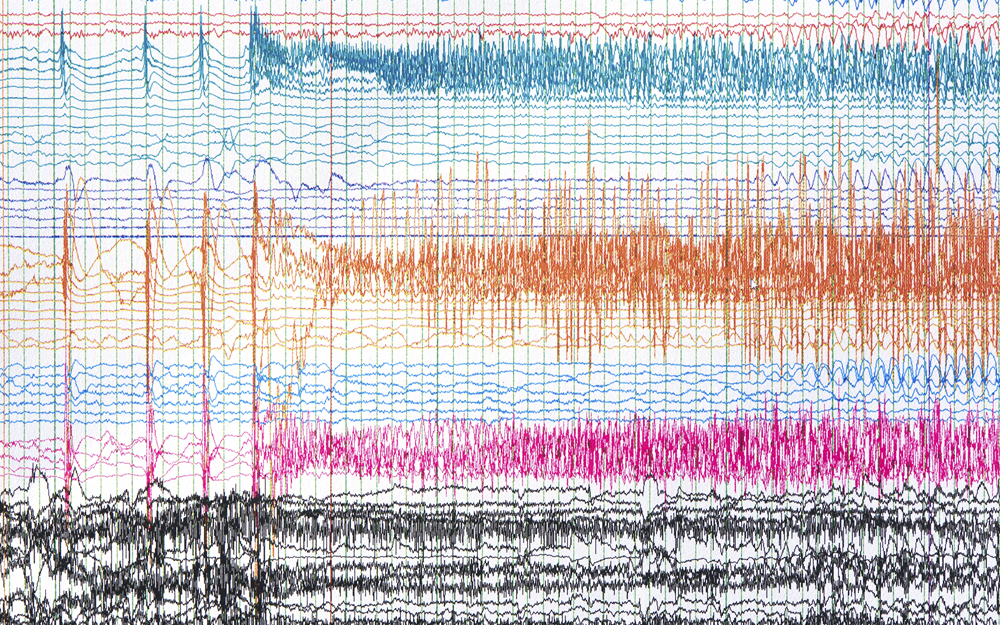
Specialists use imaging including CT scans and MRIs to find malformations and learn more about their architecture. Catheter angiograms are also used to study specific arteries from the inside.
Your doctor should especially consider imaging for:
- Young children born with skin abnormalities
- Persistent headaches not getting better with treatment
- Unusual, unexplained neurological symptoms including weakness or dizziness
- Family history of seizures or bleeding in the brain
Minimally invasive surgery and treatment options
The care plan "depends on a balance of benefit versus risk," Dr. Gonzalez adds. It might require more than one treatment.
Your provider will consider your age, medical condition and the lesion’s structure, size and location—which helps predict the malformation's chances of bleeding, stroke or serious neurological effects, as well as likely surgical outcomes or effects on surrounding essential brain tissue.
Many vascular lesions only need observation, while high-risk cases are treated with a range of surgical, radiosurgical and endovascular procedures.
Dr. Gonzalez stresses that your care team is there to help you understand your condition, resolve any fear and choose the right treatment approach.
Surgeries are done with microscopic precise surgical techniques, elaborate planning and intraoperative monitoring to preserve the normal structures of the brain and spinal cord while removing the tangles of abnormal vessels. The main advantage of surgical procedures is that they immediately eliminate hemorrhage risk from the lesion.
Endovascular embolization is a minimally invasive procedure using a catheter to enter the patient's arteries and close maldeveloped blood vessels. It works particularly well for fistulas, and as an add-on therapy for open surgery and radiation of AVMs, Dr. Gonzalez notes.
Another effective, minimally invasive option is radiosurgery ablation. The outpatient radiation treatment targets the vascular abnormality with sophisticated computer programs that precisely radiates the site of the abnormality. Treatments are done with meticulous planning and take around one hour. For larger malformations, treatment can be broken up into multiple lower-dose sessions.
The drawback of radiation?
"Radiation is a process that takes time," he warns—sometimes over the course of two to five years to experience the full effect.