Treatments for COVID-19: Know Your Options
Date
January 31, 2022

Date
January 31, 2022
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Thanks to the COVID-19 pandemic, medical terms that used to be obscure—such as monoclonal antibodies and antiviral drugs—are becoming common vocabulary. What are monoclonal antibodies? Can you ask for them if you get COVID-19? What about antiviral drugs, which are also in tight supply but can keep some people out of the hospital? Who decides which patients receive treatment?
"We've developed rigorous criteria to make sure we're administering these treatments in a way that is medically appropriate, ethical and fair."

Cedars-Sinai was one of the first medical centers in Southern California to offer COVID-19 therapies, so we spoke to Hai Tran, Cedars-Sinai Pharmacy associate director, to learn more.
What are monoclonal antibodies (MABs), and how do they work?
Hai Tran: A monoclonal antibody is a protein that's made in the lab but works like the antibodies that are made by your immune system when it's fighting an infection.
To create MABs that could fight the virus that causes COVID-19, scientists isolated immune cells from people who had successfully recovered from the illness and cloned those cells in the lab. Most of the monoclonal antibodies for COVID-19 target the spike protein, which the coronavirus uses to enter your cells.
By binding to the spike protein, the MABs can stop the virus from entering more and more cells. The goal is to help people with COVID-19 have milder symptoms and get better faster, while preventing the illness from getting worse.
Is the science new?
HT: Before the pandemic, monoclonal antibody treatments had already been used for certain viruses, such as Ebola, and for some chronic illnesses including rheumatoid arthritis and multiple sclerosis. Researchers are also working on monoclonal antibodies to fight cancer cells. So, the science isn't new, but it's definitely evolving due to the pandemic.
What about antivirals?
HT: Like monoclonal antibodies, the point of antivirals is to stop COVID-19 symptoms from getting serious and to help patients recover faster. They suppress the ability of the virus to keep multiplying in your body.
Antivirals are sometimes delivered as a combination of drugs that have different mechanisms of action. Paxlovid, a COVID-19 antiviral, is an example. It consists of nirmatrelvir—which stops the virus from making copies of itself in your body—and ritonavir, which slows down nirmatrelvir's breakdown to help it stay in the body for longer.
We've heard about so many potential therapies that it has gotten confusing. Can you give us a list of COVID-19 treatments that are currently available?
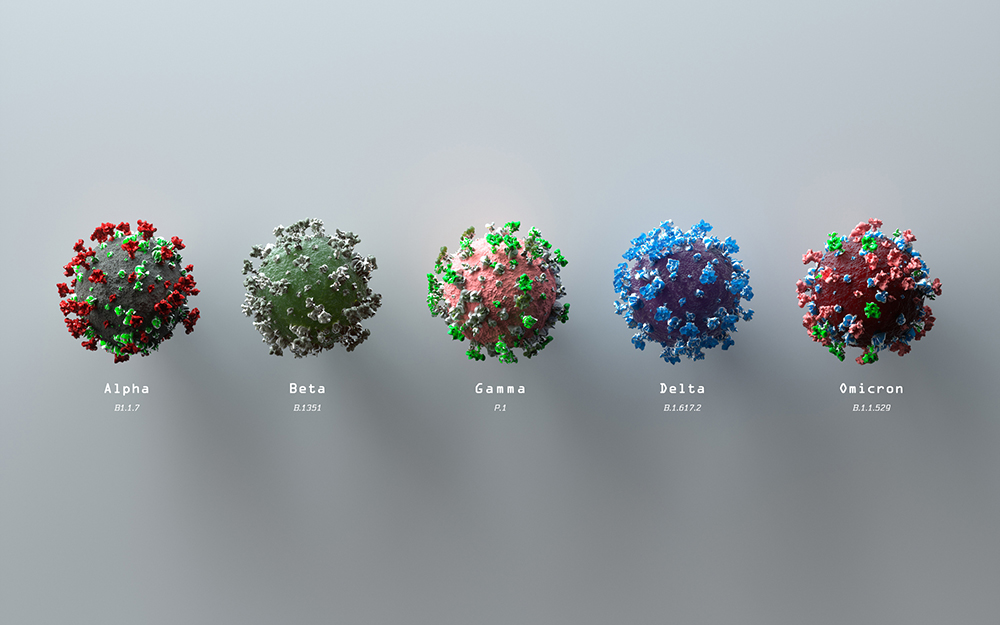
HT: It can seem bewildering, not least because it's changed over time due to evolving data and the rise of new variants. For example, we used the Regeneron monoclonal antibody treatment for certain patients until recently, but public health agencies have noted that it doesn't work against the Omicron variant.
Right now, because almost all new cases are due to Omicron, there are four therapies for people who have a mild-to-moderate COVID-19 symptoms. Sotrovimab is given through an intravenous (IV) infusion. Depending on their needs, patients can be treated either at our Ambulatory Infusion Center, at an affiliated site or at home.
The antiviral drug Paxlovid comes in pill form, as does molnupiravir. Patients take those drugs at home. Although Cedars-Sinai physicians can prescribe Paxlovid and molnupiravir, we don't have access to them at the medical center due to restricted distribution, so doctors send the prescriptions to community pharmacies.
And finally, some patients can receive remdesivir, which is an antiviral and the only COVID-19 therapy with full approval from the Food and Drug Administration and not just emergency use authorization. At first, remdesivir was only for patients who were hospitalized due to COVID-19. It has recently been authorized also for people who have mild-to-moderate symptoms and don't require hospitalization.
If a patient is eligible for sotrovimab and Paxlovid, but those therapies are not available, they qualify for remdesivir. It is administered as an IV infusion in our Ambulatory Infusion Center and is as effective as sotrovimab and Paxlovid.
Besides vaccines, are there drugs that can prevent COVID-19?
HT: The arrival of Evusheld was a breakthrough in the fight against COVID-19 because in some people, it might potentially prevent infection. It's meant for high-risk patients whose immune systems can't mount a proper response from the vaccine, or who had a life-threatening reaction to prior vaccination. Evusheld is given as an injection, not an IV, and is administered in our Ambulatory Infusion Clinic.
In the Newsroom: Why It's a Bad Idea to Try and Get COVID-19
Who is eligible for these different therapies? Can patients ask for them?
HT: With the exception of Evusheld, COVID-19 therapies are for patients who are already infected with the coronavirus. Sotrovimab, Paxlovid, molnupiravir and remdesivir are used for patients who have mild-to-moderate symptoms and are at high risk of progressing to severe illness.
With the exception of remdesivir, these therapies are in very limited supply, and the resources needed to administer them are limited, too. We've developed rigorous criteria to make sure we're administering these treatments in a way that is medically appropriate, ethical and fair.
How do you make sure the system is fair?
HT: Working with the COVID-19 Therapeutics Committee, Cedars-Sinai has developed a special risk-scoring algorithm. Age is important, as are preexisting conditions. Every order is individually assessed by the Pharmacy team and reviewed by the COVID-19 Therapeutics Panel.
As defined by the Centers for Disease Control and Prevention, preexisting conditions include immunosuppression, diseases of the heart or lungs, sickle cell disease, obesity, neurodevelopmental disorders and several others.
Can you give us an example of how you assess a patient to determine if they're eligible?
HT: Let's say you are 75 years old. Your age puts you at heightened risk. Add heart disease to the calculations, and your risk increases. But someone who is 20 years younger than you could still be in greater danger.
Based on age alone, a 55-year-old's risk is lower than yours, but if they're also facing end-state renal disease, diabetes, hypertension and chronic respiratory disease, they will be prioritized. Getting it right means understanding each patient's individual situation.
What should patients expect if they're getting treatment?
HT: Patients who are receiving sotrovimab, remdesivir or Evusheld are treated in a designated area of the Ambulatory Infusion Center, at an affiliated site or at home. In our clinic, we've made the experience as safe, comfortable and efficient as possible. The oral therapies Paxlovid and molnupiravir are picked up by the patient at a community pharmacy and taken at home.
In the Newsroom: COVID-19 Can Trigger Self-Attacking Antibodies
Do you have any advice for our readers?
HT: Ask your provider or pharmacy for fact sheets so you can familiarize yourself with these treatments. But remember that the best treatment for COVID-19 is prevention. Nothing is as good as not getting sick in the first place, so get your COVID-19 shots and your booster.


.jpg)