Why Atrial Fibrillation Can Go Unrecognized and Untreated
Date
September 23, 2022

Date
September 23, 2022
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
Traditionally considered a disease of white men over age 60, atrial fibrillation (AFib)—an irregular heart rhythm originating in the top chambers of the heart—is actually the most common heart rhythm problem across all races and sexes. It affects an estimated 5 million Americans, and experts expect that number to skyrocket to more than 12 million by 2030.
Studies suggest that AFib is most prevalent in white patients, but the fallout from AFib may be more pronounced among women, African Americans and Latinos than currently reported.
We asked Dr. Archana Ramireddy, a cardiac electrophysiologist at the Cedars-Sinai Smidt Heart Institute, to guide us through the basics of AFib and explain why the condition is underrecognized and undertreated in women and minority groups.
{{providers}}
“If you look at the prevalence of AFib in the population, men appear to have a 1.5 times higher risk than women. But since women live longer than men and tend to develop AFib 10 years later than men, AFib actually affects more women than men.”
What is AFib?
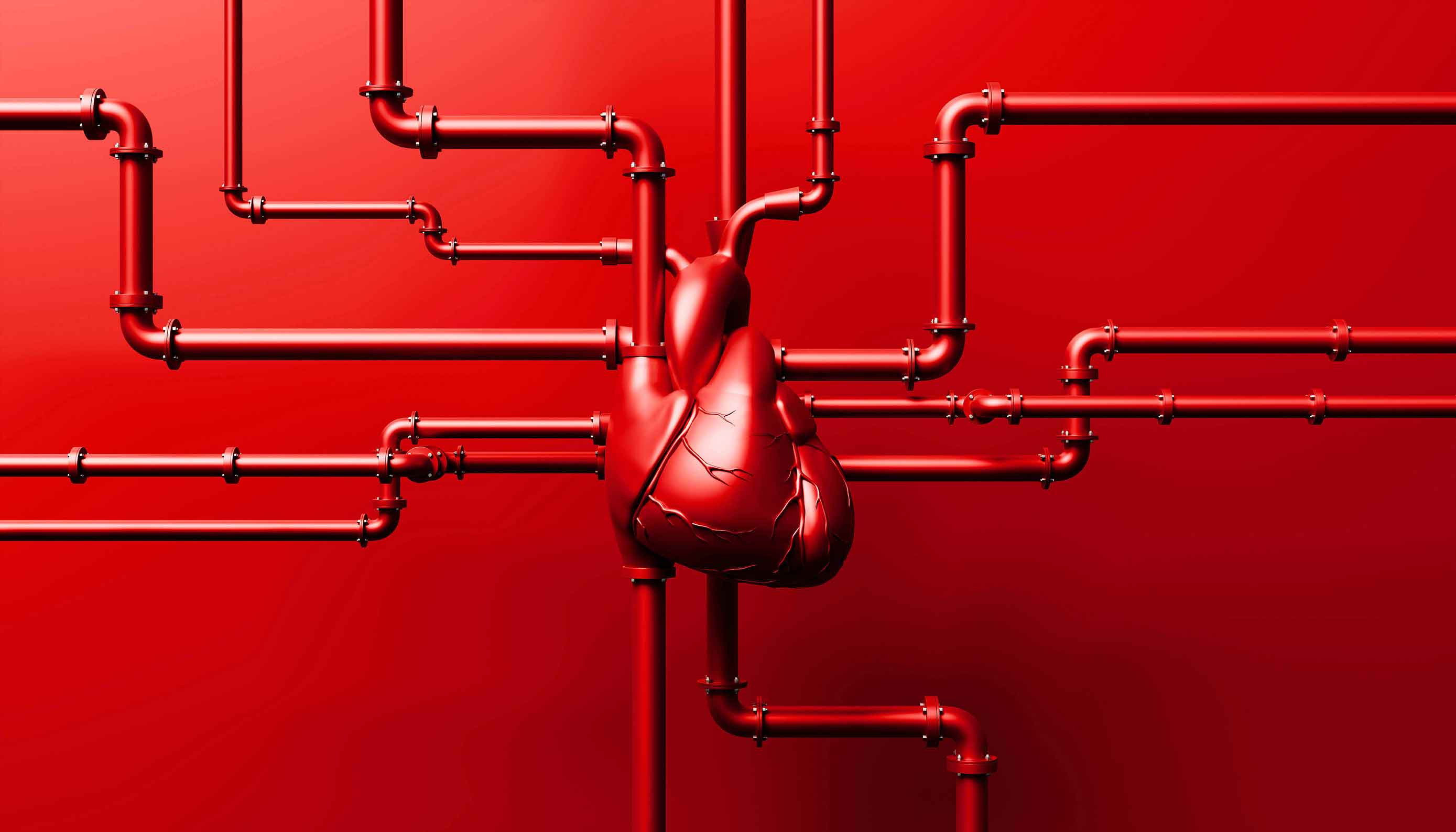
With normal heart function, the muscle fibers in the upper chambers of the heart (the atria) contract and pump blood out of the heart’s upper chambers into the lower ones (the ventricles).
In AFib, disordered or rapid electrical signals cause the heart’s atria to contract in a chaotic fashion (fibrillate). Unfortunately, blood that is not completely emptied into the lower chambers can pool in the atria. This can lead to the formation of blood clots, which can go to the brain and cause a stroke.
Risk factors for AFib include:
- High blood pressure
- Structural heart disease
- Thyroid disease
- Obesity
- Diabetes
- Sleep apnea/lung disease
- Alcohol use
- A family history of AFib
- Age (people over age 60 are at an increased risk of developing AFib)
AFib can happen in periodic episodes—particularly after drinking alcohol, a stressful event (think car accident or surgery) or acute infection (think sepsis or SARS-CoV-2, the virus that causes COVID-19)—or it can be persistent. Left untreated, AFib can lead to a host of complications ranging from blood clots and stroke to heart failure and, rarely, even a heart attack.
Studies show that such complications disproportionately strike women and minority groups. In fact, women, African Americans and Latinos with AFib have 1.5 to 2 times the risk of stroke and heart attack as white men with AFib. Yet, women and minority groups also are less likely to receive care—and lifesaving medications—for AFib than white men.
How is AFib different in women?
AFib is increasingly recognized as a condition that affects women. The trouble is most studies on AFib are made up of samples that primarily include white men.
“If you look at the prevalence of AFib in the population, men appear to have a 1.5 times higher risk than women,” Dr. Ramireddy says. “But since women live longer than men and tend to develop AFib 10 years later than men, AFib actually affects more women than men.”
In fact, Cedars-Sinai researchers published a study in JAMA Cardiology showing that women have a 50% higher risk of developing AFib than men, after accounting for height (the taller a person is, the greater their risk of AFib).
To complicate matters, women present with different symptoms than men. Instead of heart palpitations and shortness of breath (more commonly signs of AFib in men), women may feel weak, faint and lightheaded. As a result, women may not seek medical attention until their AFib has progressed. And unlike men with AFib, who typically have coronary artery disease, women with AFib often have high blood pressure and valve disease.
“Women are also more likely than men to have paroxysmal atrial fibrillation, meaning AFib that starts and stops without warning,” Dr. Ramireddy says.
“Unfortunately, paroxysmal AFib can be harder to diagnose because doctors can’t always catch it on a heart monitor, and women with an erratic or irregular heartbeat are less likely to be referred to a specialist compared to men.”
How is AFib different in minority groups?
While population-based studies typically report a lower burden of AFib in African Americans and Latinos, those communities have a higher incidence of risk factors for AFib, including obesity, high blood pressure and diabetes.
Called the AFib paradox, this discrepancy can result from several factors:
- Minority populations are underrepresented in studies. Only 44% of clinical trials on AFib break down the data by ethnicity. Among those that do, African American and Latino populations are grossly underrepresented.
- Minority populations have less access to healthcare, and they’re less likely to see a doctor for symptoms, so AFib may go undiagnosed in these populations.
- White people tend to outlive African Americans and Latinos, so minority populations may not live long enough to develop the condition (survival bias).
Proactive treatment for AFib
No matter your race or sex, you can reduce your risk of developing AFib and associated complications with lifestyle changes:
- Eat a healthy diet that includes plenty of fruits, vegetables, legumes, nuts and seeds.
- Exercise regularly and take steps to reduce your stress levels.
- Abstain from regular alcohol use.
- Work with a professional to keep your blood pressure and cholesterol levels within the normal range.
“Risk reduction is critical for everyone,” Dr. Ramireddy says. “When you lose weight, avoid alcohol, and treat chronic conditions like hypertension, diabetes, and sleep apnea, you dramatically lower your risk of AFib.”
Are you already suffering from an erratic heartbeat? A variety of medications can help control your heart rate (beta blockers) and rhythm (antiarrhythmics) as well as reduce your risk of stroke (anticoagulants).
You may also be a candidate for a procedure called catheter ablation, which uses either heat or cold to destroy tissue in the heart and disrupt the faulty electrical signals that cause the arrhythmia.