Tricuspid Valve Repair Surgery
What is tricuspid valve repair?
The heart has four valves. These valves are made of flaps that work together to open and close. This helps blood flow through the heart and out to the body. The valves promote forward flow and prevent backflow. The tricuspid valve lies between the right atrium (right upper chamber) and the right ventricle (right lower chamber).
When the flaps don’t close correctly, blood leaks back into a chamber of the heart instead of moving forward. When this happens between the right atrium and right ventricle, this condition is called tricuspid regurgitation.
When the flaps don’t open enough, blood is forced through too small an opening. When this happens between the right atrium and right ventricle, this condition is called tricuspid stenosis. This condition is rare. It often occurs with other valve abnormalities.
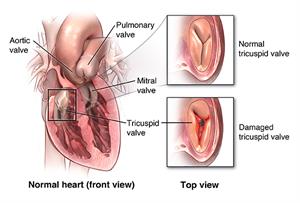
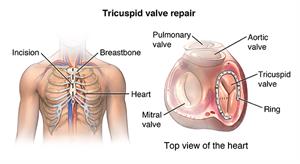
Causes of tricuspid valve problems include birth defects, rheumatic fever, and infection. They also include left ventricular heart failure, pulmonary hypertension, and changes that come with aging. Surgeons can use several methods to fix a leaking valve. These include attaching bands to support the valve, inserting rings around the valve base (annulus), and using certain types of stitches to help the valve flaps work better.
Surgeons may repair the valve with open-heart or minimally-invasive surgery.
Why might you need a tricuspid valve repair?
You may need a tricuspid valve repair if your valve is leaky or doesn't open and close correctly. You may need this surgery to correct a birth defect. Or you may need it to correct damage to the valve from endocarditis. This is an infection of your heart tissue. When the problem is just with the tricuspid valve, successful valve repair could help you regain energy and endurance. However, isolated repair of the tricuspid valve alone is rare. Surgeons often repair this valve during another planned heart surgery.
What are the risks of a tricuspid valve repair?
Tricuspid valve repair needs general anesthesia. This means you will be put to sleep and won't feel pain during the surgery. Any general anesthesia has the risk of heart or brain injury. Major surgery also carries the risk of blood clots forming during or after surgery. These clots can break free and travel to your lungs (causing a pulmonary embolism), to your brain (causing a stroke), or block blood flow as the clot becomes lodged in other blood vessels.
Other risks of the surgery include:
- Bleeding, which may need transfusions.
- Infection.
- Pneumonia.
- Damage to nearby organs, tissues, or nerves.
- Scarring.
- Heart infection (endocarditis).
- Reaction to medicine.
- Irregular heartbeats (arrhythmias).
- Heart block, requiring a pacemaker.
- Valve replacement because valve cannot be repaired.
- Heart failure.
- Death.
There may be other risks, depending on your specific health condition. Discuss any concerns with your doctor before the surgery.
How do you get ready for a tricuspid valve repair?
Before the surgery, your doctor will evaluate your health condition. Your surgeon will use echocardiogram and cardiac catheterization to find out how your tricuspid valve is working. These tests also help in planning for your surgery. An echocardiogram is an ultrasound of the heart to look at the valve and heart muscle function. Cardiac catheterization is a test done to look at blood flow through the arteries of the heart muscle. It also measures the pressure inside of the heart and the lungs.
- Your doctor will explain the surgery. Talk with your doctor about any questions you may have.
- You'll sign a consent form that gives your permission to do the surgery. Read the form carefully. Ask questions if something is not clear.
- Your doctor may do a complete physical exam. This is to make sure you're in otherwise good health before having the surgery. You may have blood tests or other diagnostic tests.
- Follow any directions you're given for not eating or drinking before surgery.
- You may be asked to shower the night before surgery or the morning of surgery using an antibacterial scrub. This is to prevent infection of the incision sites.
- Tell your doctor right away if you're pregnant or think you could be.
- Also tell your doctor:
- If you're sensitive to or are allergic to any medicines, iodine, latex, tape, or anesthesia (local and general).
- About all prescription and over-the-counter medicines you take. Also tell them about any vitamins, herbs, and supplements that you're taking. You may need to stop taking certain medicines before your surgery. Follow your doctor's instructions about which medicines need to be stopped and when.
- If you have a history of bleeding disorders. Tell them if you are taking any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may be told to stop some of these medicines before the surgery. Your doctor may request a blood test before the surgery to find out how long it takes your blood to clot.
- If you have a pacemaker or other implanted cardiac devices.
- If you smoke, quit as soon as possible before the surgery. This may improve your chances for a successful recovery from surgery. And it can benefit your overall health.
Based on your condition, your doctor may have other instructions for you.
What happens during a tricuspid valve repair?
Heart valve repair surgery often needs a hospital stay. The type of surgery you have may depend on your condition and your surgeon’s practices. Generally, heart valve repair surgery follows this process:
For open-heart surgery
- You'll be asked to remove any jewelry or other objects that may interfere with the surgery.
- You'll change into a hospital gown and empty your bladder.
- You will get an I.V. (intravenous) line in your arm or hand. You may be given I.V. antibiotics before the surgery starts.
- Other tubes (catheters) may be inserted in your neck and wrist to keep track of the status of your heart and blood pressure, and to take blood samples. Catheters may also be inserted under the collarbone and the groin.
- The anesthesiologist will keep track of your heart rate, blood pressure, breathing, and blood oxygen level during the surgery. Once you're sedated, a breathing tube will be inserted through your throat into your lungs. You'll be connected to a breathing machine (ventilator). This will breathe for you during the surgery.
- A nurse will insert a catheter into your bladder to drain urine.
- Your surgeon will insert a transesophageal echocardiogram probe into your esophagus. This is done to view the valve function after repair.
- A member of the surgical team will clean the skin over the surgical site with an antiseptic solution.
- The surgeon will make a cut (incision) down the center of the chest.
- The surgeon will divide the sternum (breastbone) in half lengthwise with a special operating tool. The two halves of the breastbone will be separated and spread apart to expose the heart.
- To do this delicate valve repair, your surgeon will need to stop your heart. Before stopping your heart, tubes are inserted into the heart so that the blood can be pumped through your body by a cardiopulmonary bypass machine.
- Once the blood has been diverted into the heart-lung bypass machine for pumping, the surgeon will stop your heart by injecting it with a cold solution.
- When your heart has stopped, the repair will start. The surgery done will depend on the type of valve problem you have. For instance, separation of fused valve leaflets, repair of torn leaflets, or the reshaping of valve parts so they work better.
- Once the surgery is done, your surgeon will allow the blood circulating through the bypass machine to re-enter your heart. They'll shock your heart with small paddles to restart its electrical activity. Slowly, your heart will resume pumping blood through your body. Your surgeon will remove the tubes connecting you to the heart-lung machine.
- Once your heart is beating again, the surgeon will check the function of the heart and the valves.
- Your surgeon may insert temporary wires for pacing into your heart. These wires can be attached to a pacemaker. Your heart can be paced, if needed, during the initial recovery period.
- Your surgeon may insert tubes into your chest to drain blood and other fluids from around the heart. These tubes will be connected to a suction device to drain fluids away from the heart.
- Your surgeon will connect the sternum back together.
- Your surgeon will sew the skin over the sternum back together and close it with stitches or staples.
- A tube may be inserted through your mouth or nose into your stomach to drain stomach fluids.
- A sterile bandage or dressing will be applied.
For a minimally invasive surgery
Your surgeon may do a minimally invasive surgery. For this, they'll insert special tools into your chest through several smaller incisions, rather than one large incision. These tools will contain a camera, as well as all the tools needed to fix your valve. This surgery might take longer than traditional open-heart surgery. But recovery may be easier.
What happens after a tricuspid valve repair?
In the hospital
- After the surgery, a member of the surgical team will take you to the recovery room or the intensive care unit (ICU). You'll be closely watched for a few days. A nurse will connect you to monitors that will constantly display your electrocardiogram tracing, blood pressure, other pressure readings, breathing rate, and oxygen level. Heart valve repair surgery generally needs a hospital stay of several days or longer.
- You may have a tube in your throat connected to a ventilator until you're stable enough to breathe on your own. As you wake up from the anesthesia more and start to breathe by yourself, your doctor will adjust the breathing machine. This is to allow you to take over more of the breathing. When you're awake enough to breathe completely by yourself and are able to cough, your doctor will remove the breathing tube. They may also remove the stomach tube at this time.
- After the breathing tube is out, your nurse will help you cough and take deep breaths every few hours. This will be uncomfortable due to soreness. But it's very important that you do this. It will help keep mucus from collecting in your lungs and possibly causing pneumonia.
- You'll be given pain medicine if you're hurting. Ask for the medicine before you become extremely uncomfortable. Your nurse will show you how to hug a pillow tightly against your chest while coughing. This helps to ease the discomfort.
- You may get special I.V. medicines to help your blood pressure and your heart rate and to control any bleeding problems. As your condition stabilizes, these medicines will be slowly decreased and turned off as your condition allows.
- Once the breathing and stomach tubes have been removed and your condition has stabilized, you may start liquids to drink. You can add more solid foods as you can handle them.
- When your doctor determines that you're ready, you'll be moved from the ICU to a post-surgical unit or acute care unit. Your recovery will continue to progress. Your activity will be slowly increased as you get out of bed and walk around for longer periods.
- Arrangements will be made for a follow-up visit with your doctor.
At home
Once your care team feels that you've recovered, you'll be discharged and may go home. Follow all your instructions for medicines, pain control, diet, activity, and wound care. Your doctor might prescribe blood-thinners to help prevent blood clots. Make sure you understand how to take them or how these medicines might affect your health and lifestyle choices. Keep all your follow-up appointments.
Other common instructions after surgery include:
- Walk at least a few times a day for as long as you can.
- Don't do any heavy lifting. Your doctor will give you a specific timeline for lifting restrictions.
- Slowly resume your normal activities as much as possible. Ask your doctor when you can go back to work and when you can have sex.
- Know that you won't be able to drive a car for some time after the surgery. This is to allow for healing of the breastbone (sternum) and the chest wall muscles. Plan to have someone give you a ride home from the hospital. Ask your doctor when you can start driving again.
- Watch your wounds for any sign of swelling, redness, bleeding, or discharge. Report these to your medical and surgical team.
- Tell your doctor about any increasing pain, fever, chest pain, or shortness of breath.
- Eat a heart-healthy diet and stay at a healthy weight. Eat foods that are low in salt, cholesterol, and fat. Try to eat a diet rich in fruits, vegetables, and lean meats.
- Don't smoke. Stay away from secondhand smoke and all other tobacco products, including electronic cigarettes.
If you need dental work in the future, your doctor may give you antibiotics to prevent infection of your valve. Before you have any dental work, always tell your dentist you've had valve surgery.
Your doctor may suggest that you begin a cardiac rehab (rehabilitation) program. This program slowly reintroduces you to a normal lifestyle. Cardiac rehab starts in the hospital with simple walking. It progresses to a regular exercise routine and a nutritious diet. Committing to healthier habits can prevent future heart problems.
Next steps
Before you agree to any test or procedure make sure you know:
- The name of the test or procedure.
- The reason you are having the test or procedure.
- What results to expect and what they mean.
- The risks and benefits of the test or procedure.
- What the possible side effects or complications are.
- When and where you are to have the test or procedure.
- Who will do the test or procedure and what that person’s qualifications are.
- What would happen if you did not have the test or procedure.
- Any alternative tests or procedures to think about.
- When and how you will get the results.
- Who to call after the test or procedure if you have questions or problems.
- How much you will have to pay for the test or procedure.
Connect with providers for illnesses like flus, UTIs and rashes (ages 3+) or chronic conditions like asthma, weight management and diabetes (ages 18+).
Cedars-Sinai has a range of comprehensive treatment options.

