Being Patient: The Delicate Timing of Organ Transplantation
Date
February 15, 2021

Date
February 15, 2021
Medical providers featured in this article
In Brief
{{cta-block}}
ORGAN TRANSPLANTATION INVOLVES WAITING, RUSHING … AND WAITING AGAIN. THERE’S THE LONG DELAY FINDING A DONOR ORGAN, THE RACE TO HAVE THE TRANSPLANT, THEN A LIFETIME OF ANTIREJECTION MAINTENANCE. ALL THROUGH THIS EXTENDED JOURNEY, CARE TEAMS ARE MONITORING PATIENTS’ HEALTH TO ENSURE THEIR SURVIVAL.
Six months after getting married, Patrick Han learned his kidneys were failing. A longtime Angeleno, he braced himself for the delay shared by many patients wait-listed for kidney transplants in California: an average of 10 to 12 years. While waiting, deteriorating health forced him to quit his job at a pro golf shop.
His condition had a ripple effect on his loved ones, too. His wife had been studying for her doctorate in psychology.
"It's heartbreaking to tell families they have to wait."
– Irene Kim, MD
"We tried to live normally for as long as we could," says Jessica Han, but to cope with her husband's mounting care needs, she eventually quit school.
Transplant surgeries have a complex relationship with time. Wait times can be long—while the need for an organ is urgent. Cedars-Sinai transplant teams help patients sensitively navigate this frustrating balance of "hurry up and wait." But once a matching organ is found and transplanted, the consequences can be profoundly life-altering.
"Nowhere else in medicine do you see someone with one foot in the grave literally walk out the front door with a new heart and a new lease on life. That's quite extraordinary," says Jon Kobashigawa, MD, associate director of the Smidt Heart Institute and director of the Advanced Heart Disease Section as well as the Heart Transplant Program.
Checkpoint 1: The Long Wait for an Organ
Being Patient
A series of critical checkpoints must be navigated along the way to organ transplantation. While awaiting his trans- plant, Han had to undergo kidney dialysis. Hypertension and the long-term effects of immunosuppressant drugs from a liver transplant at age 27 had wrecked his kidneys.
Everything in his life had to be scheduled around four hours of dialysis each Monday, Wednesday and Friday, severely restricting time with family and any activities.
"Remaining on dialysis raises the risk of death compared to receiving a lifesaving kidney transplant," explains Irene Kim, MD, co-director of the Cedars-Sinai Comprehensive Transplant Center, surgical director of Kidney Transplantation and one of Han's surgeons. "Furthermore, staying on dialysis negatively impacts the quality of life."
In his 30s, Han had youth on his side. But up to 10 years on dialysis can take a devastating toll.
"If you're an older recipient," Kim says, "it literally is a race against time to get transplanted."
Han's parents volunteered to be kidney donors. Given their age, he rejected their offers out of concern for their health. His wife and one of her friends were also willing donors. Neither was a match, adding heartache to an already difficult situation. The uncertainty of an unknown wait time took a heavy emotional toll.
"I was in a dark place," Han says. All the family could do was wait, and hope, for a life-changing organ donation.
Organ Systems
Patients awaiting organ transplantation get listed in an organ-matchmaking database administered by the non- profit United Network for Organ Sharing (UNOS). The UNOS computer system matches donors with potential transplant recipients by examining blood type, organ size, wait time, geography, medical urgency, age and degree of immune-system compatibility.
While well-intentioned, the UNOS system has some drawbacks that can lead to frustration and prolonged wait times, says Andrew Klein, MD, director of the Division of Transplant Surgery and co-director of the Cedars-Sinai Comprehensive Transplant Center, and the Esther and Mark Schulman Chair in Surgery and Transplantation Medicine.
UNOS divides the United States into 11 regions and 60 local areas. Procured organs primarily stay within local areas, but some places have more organs available than people waiting, leading to inequities for those who can't afford to travel for surgery. Such issues have prompted Klein to spearhead advocacy for national policy changes.
Regardless of the organ being transplanted, the waiting phase is tough.
"It's heartbreaking to tell families they have to wait," Kim says. "When you are listed for a kidney transplant in California, if you do not have a living donor, you are on the wait-list for up to 10 years or more."
The Benefits of an Imperfect Match
California is known nationally for its long wait times. But geography is not the only factor. Organ donors and recipients are matched by blood group (A, B, AB, O), and people of some blood types are more likely to donate than others.
That, explains Kim, is a challenge for individuals with type B blood, 70% of whom are of minority origin—including people who are Latino, Black, Asian and Pacific Islander. A reluctance by some cultures for organ donation means that patients like Han, who is Korean American, can be at a disadvantage when it comes to organ-transplantation opportunities.
Fortunately, availability of a kidney for Han was sped up through a national program that recognizes compatibility between specific type A donors and type B recipients, boosting chances of a match. Cedars-Sinai was one of the first medical centers in Los Angeles to offer this program, so Han received his donor transplant years earlier than he might have elsewhere. Not all medical centers participate in the program, explains Kim, and getting earlier access possibly saved Han's life.
ONCE AN ORGAN IS PROCURED, THE CLOCK STARTS RUNNING DOWN.

Checkpoint 2: Surgery
The Ticking Clock
For Han, six years of waiting ended with a telephone call on October 22, 2019. Cedars-Sinai had an organ match and surgeons were ready to operate.
"We had to throw every- thing together in a bag and go," Jessica Han says.
Just over an hour after receiving that life-altering phone call, the couple arrived at Cedars-Sinai. Han was whisked off to surgery. He awoke with a new kidney five hours later.
Once an organ is procured, the clock starts running down. Like the phone call that sent the Hans packing in short order, the timeline from procurement to surgery can be mere hours. For example, a heart can only stay out of the body for five to six hours before deteriorating.
"Within three hours of procurement, we want the blood to be re-perfused—pumped back into the heart," says Kobashigawa, who is also the DSL/Thomas D. Gordon Chair in Heart Transplantation Medicine.
Cutting-Edge Technologies
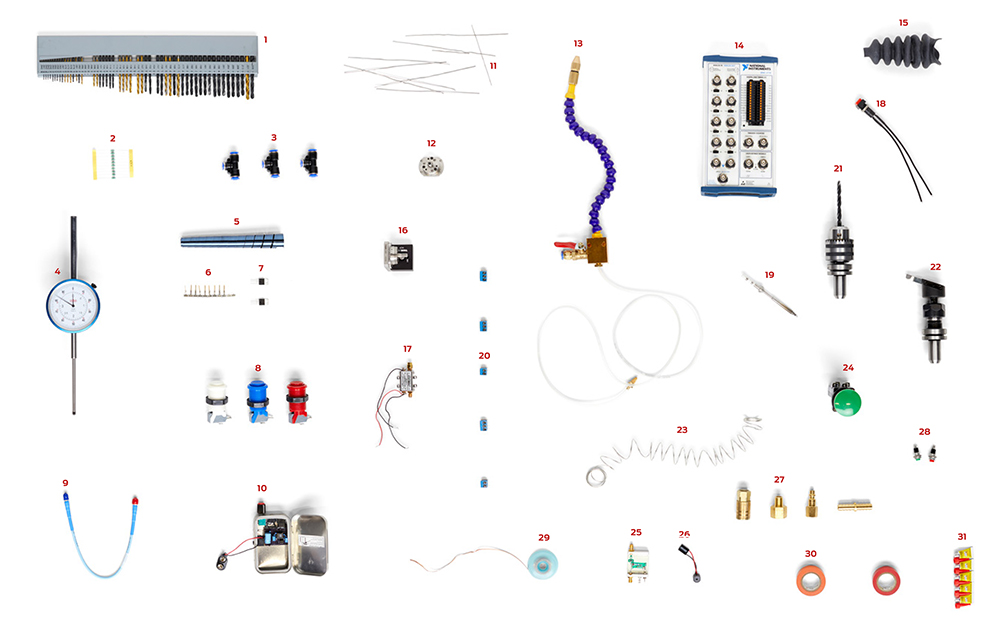
One technology that may stretch that critical time window is the organ-care system. Called "Heart in a Box," this machine is taken by the procurement team to the donor hospital.
Following removal from the body, "the heart gets re-animated, so it starts beating on this machine, as if it was in the human body," says Fardad Esmailian, MD, surgical director of Heart Transplantation and Mechanical Circulatory Support. Keeping a donor heart beating creates the potential for donor heart retrieval from greater distances than ever, including from as far away as Hawaii.
Cedars-Sinai is using this organ-care system in a new study called the Donation after Circulatory Death (DCD) Heart Trial.
After a family has agreed to withdraw life support from a family member with an irreversible brain injury, the deceased's organs are used to give life to others.
"We're hoping to increase the transplantation rate by about 20% or 30% using this kind of a device in DCD donors," Esmailian says.

Checkpoint 3: Rejection
The Immune System: Friend and Foe
It was no coincidence that the first successful kidney transplant in 1954 was between twin brothers. By the 1950s, research had established that tissues were freely interchangeable between identical twins. When donor and recipient were not genetically identical, immune rejection occurred.
The immune response is the body's defense against any foreign invader. The problem with transplants is that the lifesaving organ gets mistaken as an interloper unless the immune system is instructed to stand down. In organ transplants of the 1950s,"there were so many problems with rejection and deaths that it wasn't felt to be a very good therapy," says Stanley Jordan, MD, medical director of the Kidney Transplant Program and director of the Human Leukocyte Antigen and Transplant Immunology Laboratory. Back then, few medications were available to prevent rejection. The ones that did exist often caused serious complications.
Soldiers on the immune system's front lines are white blood cells. For decades, therapeutics focused on T cells, which are part of this army. Over time, it emerged that antibodies—immunoglobulin proteins secreted by another white blood cell type, B cells—could cause organ rejection, too.
Researchers now understand that both cellular and antibody-mediated rejection is important. So pharmaceutical approaches to antirejection chemically instruct both kinds of soldiers to stand down.
On the Horizon
Cedars-Sinai experts like Kobashigawa and Jordan have been at the forefront of research to circumvent organ rejection. Kobashigawa now leads a clinical trial for tocilizumab, a drug that may block a key step in the rejection cascade.
Jordan is also testing repurposed cancer and autoimmunity drugs. One promising lead is an unlikely ally: an enzyme called imlifidase that is derived from flesh-eating streptococcal bacteria. This enzyme acts by chopping immunoglobulin soldier molecules in half.
"These bacteria just amaze me," Jordan says. He hopes that imlifidase, now under review by the Food and Drug Administration, can allow transplants in people for whom antibody control has failed. Imlifidase was recently approved by the European Medicines Agency for desensitization in European countries, based primarily on work done at Cedars-Sinai.
Other promising therapies include artificial organs and regenerative medicine. However, the best result of any procedure—now or in the future—isn't just saving a life but improving one.
By the Numbers
{{column-start}}
286
kidney transplants performed at Cedars-Sinai in 2020
{{column-end}}
{{column-start}}
100%
of Cedars-Sinai patients—adult and pediatric—who received a kidney from a living donor had a functioning transplant after one year
{{column-end}}
{{column-start}}
66.3%
of heart transplant patients on the Cedars-Sinai wait-list received an organ within one year—compared to 54% nationally
{{column-end}}
{{column-start}}
92.3%
of kidney-pancreas patients on the Cedars-Sinai wait-list received a transplant within three years—compared to 60.4% nationally
{{column-end}}
{{column-start}}
93
Cedars-Sinai patients on the heart transplant wait-list as of March 2021
{{column-end}}
{{column-start}}
128
heart transplants performed at Cedars-Sinai in 2020
{{column-end}}