What Is Robotic Surgery? An Explanation for Patients
Date
February 11, 2026

Date
February 11, 2026
Medical providers featured in this article


In Brief
In 1985, one of the earliest robotic surgeries took place when a robotic arm assisted in a brain biopsy procedure.
Since then, robotic surgery has grown significantly and now accounts for more than 20% of all surgeries in America. But there are a lot of misconceptions about what robotic surgery is and how it really works.
Patients may wonder: What does the robot look like? Is it actually performing the operation? What’s the surgeon’s role?
We asked three Cedars-Sinai surgeons with a lot of robotic surgery experience to explain what’s really going on when they go into the operating room (OR) with the robot.
Here is an excerpt of our conversation with Dominic Emerson, MD, director of Robotic Cardiac Surgery; Curtis Cetrulo, MD, director of the Division of Plastic Surgery and the General William and Willa Dean Lyon Family Chair in Reconstructive and Plastic Surgery in honor of Randolph Sherman, MD; and urologic surgeon Andrew Hung, MD.
{{cta-block}}
Emerson: A common misconception I hear from patients is that the robot is acting autonomously—that it’s the one doing the surgery while we surgeons sit back and have coffee. And that’s not true. It is really just a tool we use in the OR, just like a scalpel or scissors.
{{providers}}
The way I explain it to my patients is that performing robot-assisted surgery is like being a puppeteer. When I move my hands, the robot does exactly what I do. It never acts independently.
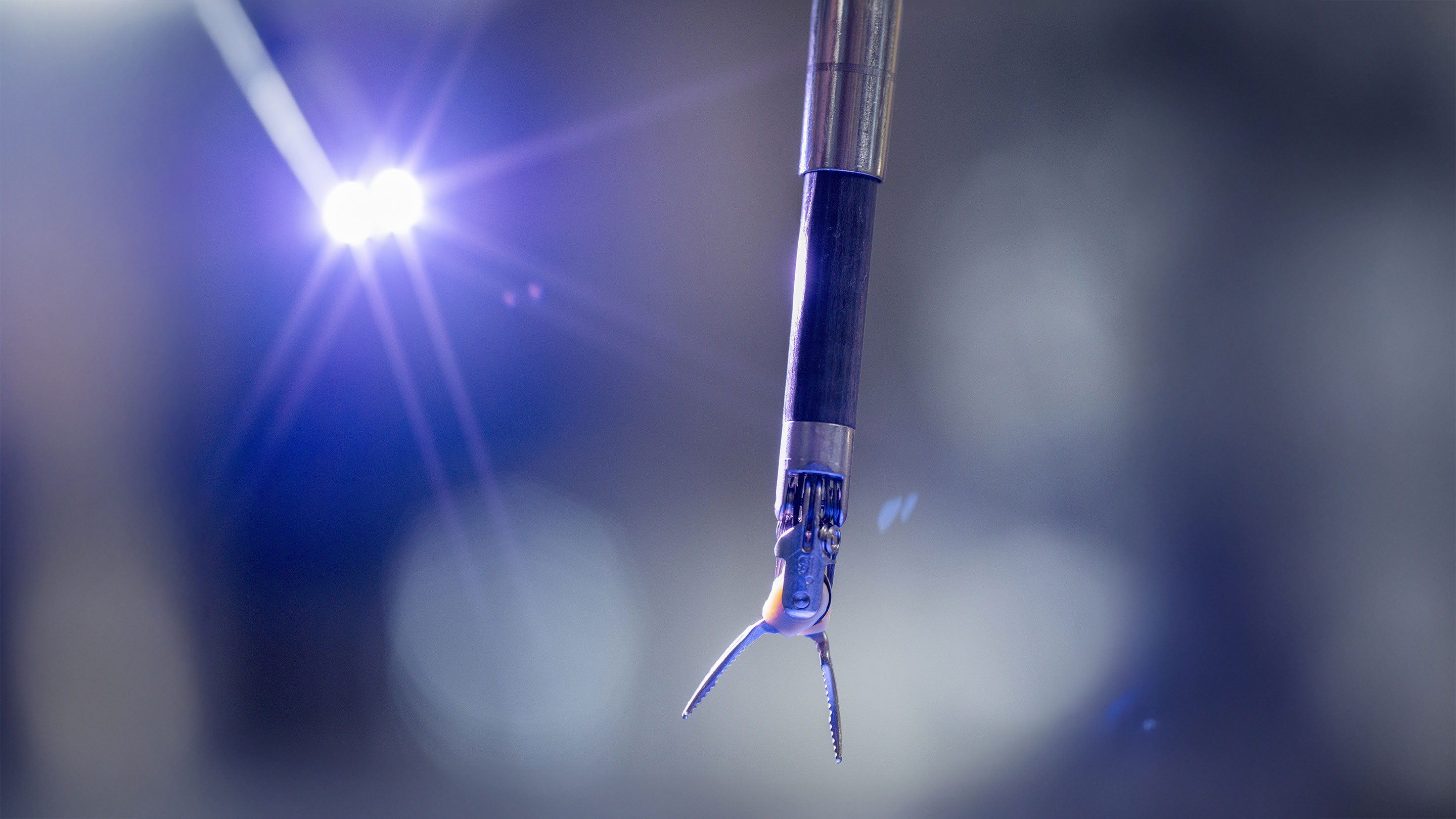
The robot is basically just four arms that hang down over the operating table. Three of the arms have surgical tools on the end and one has a camera. As the surgeon, I sit in the corner of the OR in this little pod-like thing. I look through a viewfinder, which provides a high-definition 3D image of whatever the camera on the robot sees. It’s very immersive. I have my fingers in controls that are like little pincher graspers. When I move my hand, the robot arm moves, and I can control which arm’s moving. Ultimately, the robot is not doing anything independently. It’s just doing whatever I’m doing with my hands.
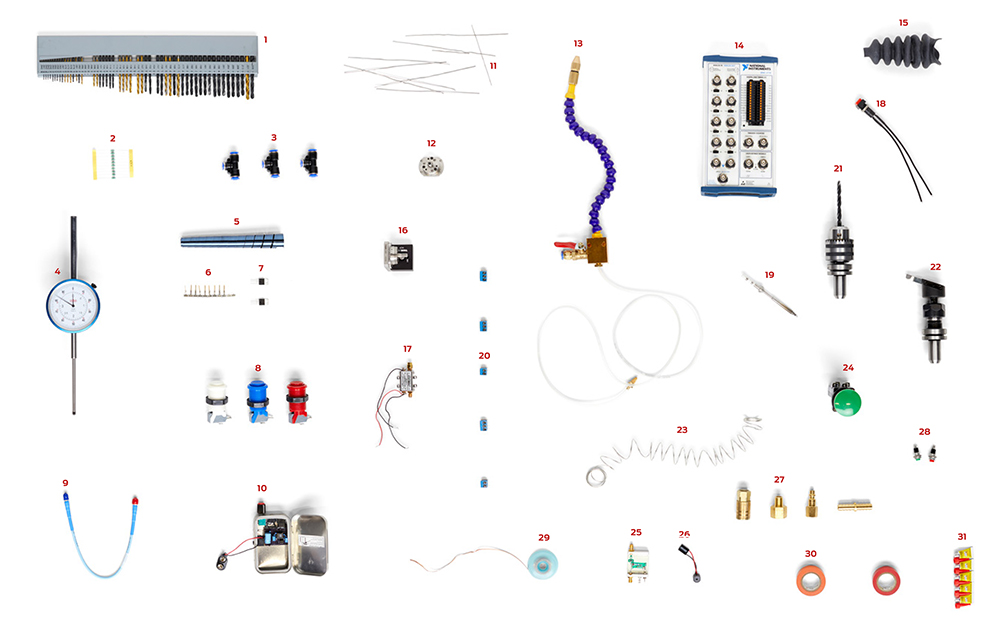
The robot arms are a little thicker than a pencil, so they can go through very small, minimally invasive incisions, much smaller than regular open surgery. And they have tools on the end, such as something you can grasp with, something to drive a needle with, scissors … there's a wealth of specialized instruments you can use. When you need a new tool, a surgical technician can switch it out in just a few seconds.
Cetrulo: I call it robotic-enabled or robot-assisted surgery, just to be clear the robot’s not doing the surgery. An important advantage of the robot is precision. I can set it up so when I move my hand a few inches, the robot makes a much smaller movement.
In microsurgery and plastic and reconstructive surgery, we often work under the microscope. We can place tiny sutures in a 1-millimeter artery or vein (roughly 1/25 of an inch) with our fingers. But how about a 0.1-millimeter lymphatic vessel (roughly 1/256 of an inch)? We can’t do that with our fingers. It’s just too fine. But we can do it when a robot scales down our movements.
The robot also dampens the tremors in our hands, because even the steadiest hands have a microtremor. So, when you put the needle in, it goes in straight and true every time, and it doesn't cause any damage or tears in the vessel.
Hung: I am a urologic surgeon, and I specialize in cancers. A prostatectomy—removing a patient’s cancerous prostate—is the most common procedure I do with the robot. A close second would be a kidney operation.
I was in surgical training right around the time when robotic surgery was starting to replace traditional open surgery, and my mentor in medical school famously told me, “You know, don’t worry about this robot thing. It’s just a fad. It’s going to go away.”
Of course, it hasn’t. In fact, robot-assisted prostate surgery has replaced open prostate surgery.
The difficulty with prostate surgery is that the prostate is deep down in the pelvis. It’s just not very easily accessed. Even with a big open incision, you really couldn’t see the prostate very well, so these operations were often done by feel.
This area of the body is where the most sensitive parts of the male reproductive tract meet the urinary tract. A lot of nerves converge here, including the nerves that control sexual function. The great thing about the robot is that not only am I making a much smaller incision, but the instruments are extremely long and the robot’s camera can zoom in. So, when I’m at the console, I can get to that spot and be staring at the prostate as if I’m right there, millimeters away from it. I can see, I can magnify, and the outcomes for patients are drastically better, in my opinion.
Cetrulo: In my whole career as a microsurgeon, I’ve been working in this tiny space looking through a keyhole with a microscope. But the camera on the microsurgery robot arm projects onto this huge high-definition screen in the OR. It’s so cool—it’s like you’re landing a plane on the artery and putting your sutures in.
We do a lot of lymphatic vessel bypass surgery, and those vessels are so small that it might take an hour to do one bypass without the assistance of the robot. But with the robot, I can do maybe three in an hour. That means a better outcome for the patient.
It’s really becoming a game-changer for a lot of microsurgical procedures.
Emerson: In cardiac and thoracic surgery—surgeries in the chest—we often use the robot to replace or repair the mitral valve and other heart valves. I’m also using it in heart bypass surgery. At Cedars-Sinai, we were the first in the world to use it for a lung transplant surgery. We did that at the end of 2021, and now more surgeons across the world are doing it that way.
Robot-assisted surgery is great for patients because it’s so much less invasive. Open-heart surgery involves something called a sternotomy, where we make a big incision and cut through the breastbone and the chest muscles to see and get access to the heart. It’s a fine way to do it, and most of these surgeries are still done that way. But with the robot, I make a much smaller incision and enter the chest in between the ribs, so there’s less blood loss and less damage to nerves and muscles, and the recovery is much quicker.
Cetrulo: Robot-assisted surgery is also easier on the surgeon. Neck problems are one of the biggest sources of disability for surgeons, because we’re leaning over the operating table for hours at a time. With the robot, everything is adjustable, so you can set yourself up to be in a good ergonomic position. That can keep surgeons active longer so they can help more patients.
Emerson: There is a learning curve. Robotic surgery uses very different technology than an open operation, so it does require additional training. That’s one of the limiting factors. Many surgeons who haven’t been trained on it prefer to stick with what they know. But as newer surgeons come into the field, that’s changing. At Cedars-Sinai, we’ve been training early career surgeons in using the robot. I’ve also helped set up several centers across the country where I go and proctor people on their first five to 10 cases.
These robotic systems are expensive, too. We have a number of them here at Cedars-Sinai, but not all surgeons and patients have access to the technology right now.
Cetrulo: In the future, remote surgery could really democratize access. Right now, the surgeon is almost always in the room. But they don’t have to be. There are cases happening with expert surgeons operating remotely on patients far away—even across the world!
Hung: Integrating AI into robot-assisted surgery is a big focus for the future. There’s a wealth of data available on most patients—such as CT scans and MRIs—and AI can help distill all that information and provide a kind of augmented reality. For example, during the operation, AI may be able to show the surgeon things about the patient’s anatomy that may not be visible, such as blood vessels or nerves that are hidden behind other structures.
Cetrulo: Right now, the robot is just an extension—a tool—for the surgeon, but automation is coming. We do a lot of simple, rote surgeries, such as carpal tunnel or trigger finger release surgeries. In the future, I think these will be automated and handled entirely by the robot. We’re not there now, but it’s coming.
Frequently Asked Questions
Is robotic surgery performed entirely by a robot?
No. Robotic surgery is fully controlled by a surgeon who directs every movement of the robotic instruments.
Is robotic surgery safer than traditional surgery?
The robotic systems used at Cedars-Sinai are approved by the U.S. Food and Drug Administration. Because they are minimally invasive—meaning they use smaller incisions than open surgery—they can offer benefits such as faster recovery. But safety depends on the procedure, the patient and the surgeon’s level of experience.
Is robotic surgery the same as artificial intelligence?
No. Robotic surgical systems do not make decisions on their own and do not use AI to operate independently.
What types of surgery can be done robotically?
Robotic surgery is used in heart, lung, urologic, abdominal, and plastic and reconstructive procedures, among others.
How do I know if robotic surgery is right for me?
A surgeon can evaluate your condition, anatomy and overall health to determine whether robotic surgery is an appropriate option.