Better Brain Surgery
Date
February 11, 2020
Credits
Date
February 11, 2020
Credits
Medical providers featured in this article
In Brief
{{cta-block}}
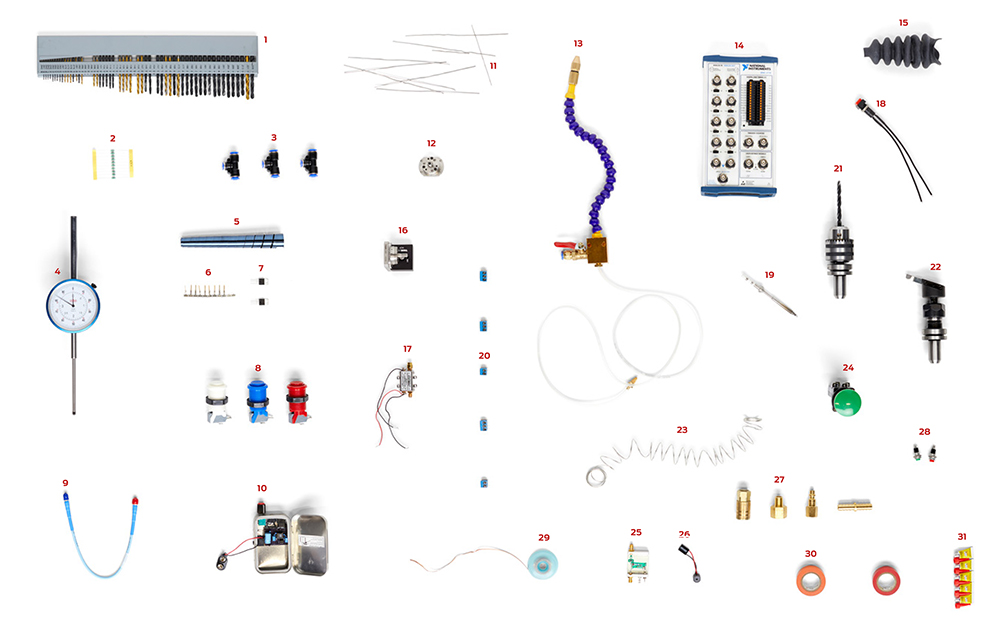
The laboratory of Pramod Butte, PhD, is chockablock with bins of computer innards, pumps, dials, "useless random fasteners," capacitors and chunky buttons begging to be pushed. Silvery metal filings frost a corner table beside a tidy row of drill bits. From such seemingly arcane items, Butte forges innovative methods to help surgeons distinguish cancerous cells from healthy ones.
Distinguishing tumors from healthy tissue
"The problem with brain surgery has been we don't know where the boundary is between tumor and normal tissue," says Butte, a research scientist in the Maxine Dunitz Neurosurgical Institute. "If you take too little, you leave tumor behind. If you take too much, you remove normal brain."
Traditionally, neurosurgeons use brain scans like MRIs to create a map they can project onto the skull during surgery.
"But the MRIs are imprecise," Butte says. "And as soon as you open the skull, the tumor shifts."
Read about the neurovascular surgery journey of The Luckiest Unlucky Kid.
SOLUTION: Light them up
Butte is helping surgeons "see" tumors using fluorescence, like "what happens with black light at the bowling alley," he explains.
When tissue is hit with ultraviolet (UV) light, it absorbs the radiation and rapidly spits back its own signal. When earning his PhD in 2002, Butte hypothesized that cancerous and healthy cells would emit different signals. He thought fluorescence could help surgeons pinpoint tumors in the operating room.
"We developed a UV laser," Butte says. "The laser flashes for 350 picoseconds." Since a picosecond is one trillionth of a second, he adds, "It's a very, very fast laser."
Butte and his team worked on designing and refining the laser for more than a decade. They also devised a machine to pick up the fluorescent signal as well as software to analyze it. (The metal filings sprinkling his lab are a byproduct of machining custom bolts and plates for the apparatus.)
Finally, a clinical trial in 2016 which included more than 250 surgical cases, tested whether his system could distinguish between tumors and normal tissue.
"The surgeon simply would point the probe, flash the laser, record the signal and later run a biopsy to test if our results matched pathology," Butte says.
Not only was his system accurate, but demonstrated the potential of the system to provide the feedback in the operating room to help direct the surgeon toward which areas to cut—and which not to—in real time.
With the brain tumor results as a proof of concept, the Butte laboratory is conducting a clinical trial with breast cancer patients. The goal is to reduce the number of repeat surgeries many women undergo after a lump is removed.