A Blood Test That Could Detect Cancers Before They Appear
Date
January 16, 2026

Date
January 16, 2026
Medical providers featured in this article


In Brief
- Large oncosomes are cancer cell-derived extracellular vesicles that can be reliably isolated from blood and carry consistent molecular signatures across multiple cancer types, making them a promising candidate for future universal blood-based cancer tests.
- This discovery helps overcome a major challenge in liquid biopsy research: the difficulty of detecting rare, tumor-derived signals amid the dense background "noise" of other materials in the blood. Large oncosomes are big enough and distinct enough to filter out.
- Blood screening for cancer could allow those who don’t qualify for current screening ,or cannot afford it, to access early cancer detection.
Blood is not a liquid, it’s a landscape—a dense cellular terrain teeming with deeply buried secrets for understanding disease.
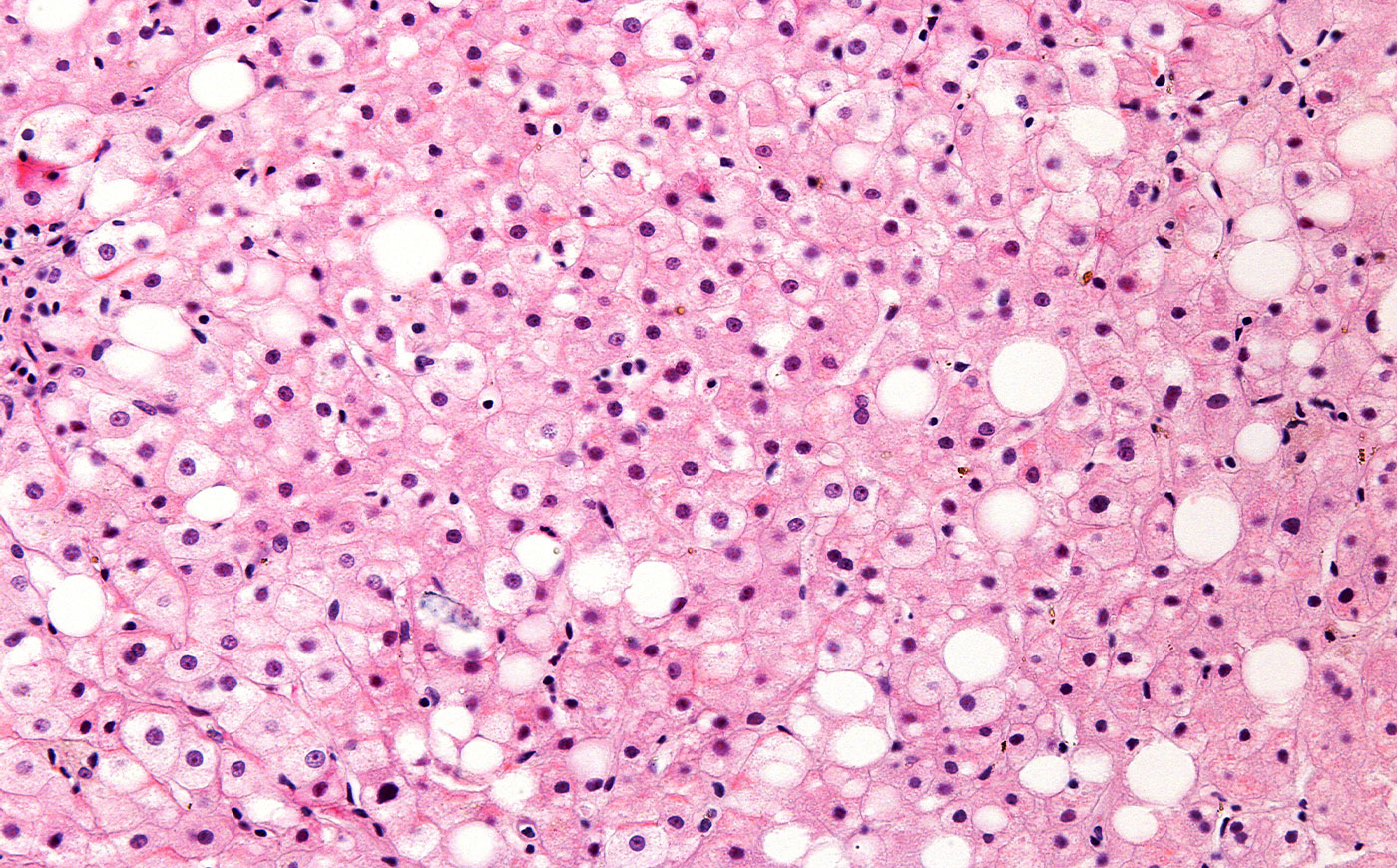
Cedars-Sinai investigators have navigated this microscopic world and made a rare discovery: a blood component that could lead to the development of liquid biopsies for cancer diagnosis, prediction and treatment.
Their research revealed that large oncosomes—vesicles cast off by tumor cells—contain a set of molecules consistent across cancer types. That makes large oncosomes more than cellular debris; they’re landmarks. By mapping them, researchers could help redraw the future of cancer care.
“This work enables us to develop strategies to separate the vesicles coming from the tumor from the rest of the particles in the blood,” said collaborators Michael Freeman, PhD, professor of Urology, director of the Division of Cancer Biology and Therapeutics Research, and the Ben Maltz Chair in Cancer Therapeutics at Cedars-Sinai; and Dolores Di Vizio, MD, PhD, a professor of Urology at Cedars-Sinai who will be transitioning to visiting professor as she continues to actively collaborate with Cedars-Sinai investigators. “Identifying these large oncosomes and better understanding them puts us on a pathway to blood tests with the ability to detect multiple cancers.”
Across cancer research, investigators are rethinking what blood can reveal, including where disease is located, how it behaves, how it changes and how it responds to treatment. This bold vision is increasingly tangible: a future in which blood tests play a crucial role in early diagnosis, monitoring and precision care.
“We are all looking to the blood as a window into people at risk for cancer, people with cancer and people who are being followed in their treatment for cancer,” said Robert Figlin, MD, interim director of Cedars-Sinai Cancer and the Steven Spielberg Family Chair in Hematology-Oncology. “The research is still in progress, but it’s progress with direction. Blood may become one of the best tools we have to track cancers we cannot yet see.”
A Promising New Biomarker
Can we detect cancer in the blood before it becomes lethal? Cedars-Sinai researchers have found their answer in large oncosomes—fluid-filled sacs released into the bloodstream by aggressive cancer cells.
A recent study from Cedars-Sinai published in Cell Reports Medicine with Di Vizio as senior author, found large oncosomes have a consistent set of molecules across cancer cell models—including brain, prostate and breast cancers—and appear in the blood of patients with metastatic prostate cancer. This unlocks the potential for a more universal screening tool.
Most blood-based markers and tests are tumor-specific. Large oncosomes could enable the development of a single blood test capable of detecting multiple cancers and discriminating among them.
“It brings us closer to true early detection, especially for people with no symptoms,” Freeman said.
Large oncosomes may help investigators overcome one of the most challenging obstacles in the liquid biopsy field: the background noise of the blood itself. Blood is densely populated with vesicles from every organ and system. Most methods that rely on extracellular vesicles are unreliable detectors because tumor-derived signals are vastly outnumbered by the other materials in the blood.
Large oncosomes are big enough to be profiled, and their surface proteins—newly identified by the investigators—offer a reliable way to filter out a whisper in a roaring crowd. The discovery opens the door to practical tools, such as clinical assays, diagnostic kits and new imaging strategies that could bring large oncosomes into routine cancer care.
Cedars-Sinai investigators have begun to validate the work in additional patient cohorts and are on the cusp of real-world clinical applications. Their immediate target is prostate cancer, with the intent to distinguish indolent from aggressive disease, avoid over treatment and unnecessary surgeries, and spot tiny metastatic sites undetectable by imaging alone.
Collaborations with clinicians at Cedars-Sinai, Massachusetts General Hospital, Harvard University and the University of Trento in Italy are ongoing, with a major 400-patient prostate cancer study. Lauren Newman, PhD, a postdoctoral scientist, is branching into lung and kidney cancer, working closely with oncologists to validate the approach across tumor types.
Investigators aim to track treatment response in clinical trials, develop a rapid-use clinical kit for oncosome detection and launch efforts to make the technology widely available.
A Blood Test You’d Actually Use
For Jane Figueiredo, PhD, professor of Medicine and director of Community and Population Health Research at Cedars-Sinai Cancer, the greatest promise of blood-based tests is to improve accessibility for patients who are not being tested. Not all cancers are amenable to population-based screening, and some at-risk patients may not qualify for it.
Colonoscopies, mammograms and similar tests are limited. Younger people, especially those under age 45, are often excluded from screening—and increasingly at risk as cancer rates continue to climb among younger people.
“There are entire populations who don’t have access to screening,” Figueiredo said. “They’re too young, they don’t meet the guidelines, they’re not insured or they’re simply not seeing their doctor.”
Figueiredo’s research focuses on building better tools for cancer prevention and early detection, especially among groups long excluded from traditional care. One blood-based approach uses polygenic risk scores—calculations based on genetic patterns that reveal the likelihood a patient will develop cancer. These scores offer a way to identify high-risk individuals before they show symptoms and before they would otherwise qualify for screening.
“It’s one pathway to personalized prevention,” Figueiredo said.
But risk detection doesn’t always translate to clinical utility. A test must be accurate and reliably lead to clinically useful strategies for prevention or mitigation.
“We believe this is where the field needs to go. You don’t want to just tell someone they’re at risk; you have to be able to do something about it,” she said.
Blood tests to predict and identify cancer are particularly efficient for patients who can't—or won't—undergo more invasive procedures.
This rich vein of research is yielding a common vision: blood as a central tool in the early detection and continuing care of cancer.
“The field is moving fast,” Figlin said. “The more we understand about blood, the more powerfully we can use it. We’re entering an era where a blood draw can offer a clearer view of cancer than we’ve ever had before.”