How AI Is Helping Predict and Prevent Cardiac Arrest and Heart Attack
Date
January 5, 2026
Date
January 5, 2026
Medical providers featured in this article


In Brief
Every year, hundreds of thousands of Americans are killed by sudden cardiac arrest (SCA) and myocardial infarction (MI).
For decades, researchers and physicians have struggled to find better ways to predict who is most at risk and the means to keep their hearts beating. Studies carried out at Cedars-Sinai are challenging these longstanding limitations to heart care, addressing risk that has historically seemed impossible to quantify.
Investigators at the new Artificial Intelligence in Medicine Research Center and the Smidt Heart Institute at Cedars-Sinai are at the vanguard of this effort. Their research has identified 13 biomarkers of SCA risk—along with a number of early warning symptoms—that stand to significantly improve early detection.
Investigators also are improving risk prediction for MI by training AI to gather more information from cardiac imaging, and in far less time, than can be accomplished by human radiologists.
These results promise a leap forward in the assessment of cardiac health.

One Biomarker Is Not Enough
Sumeet Chugh, MD, vice dean and chief artificial intelligence health research officer, director of the Artificial Intelligence in Medicine Research Center, and director of the Center for Cardiac Arrest Prevention at Cedars-Sinai, said cardiologists have depended for decades on an increasingly inadequate biomarker—low left ventricular ejection fraction (LVEF)—to determine who is most at risk for SCA and should be fitted prophylactically with an implanted cardiac defibrillator. In a study published 20 years ago in the Journal of the American College of Cardiology, Chugh found that roughly two-thirds of patients who experienced SCA did not have a severely reduced LVEF.
The work was roundly criticized, he said, but many subsequent studies have come to support its conclusions.
“We had a lot of rotten eggs thrown at us because we were undermining a vital tool in the cardiologist’s arsenal,” said Chugh, who is the Pauline and Harold Price Chair in Cardiac Electrophysiology Research. “But our results have since become gospel in the field.”
The Long Game
In 2022, Chugh and his team released a clinical tool, VFRisk, that scores a patient’s SCA risk based on 13 biomarkers drawn from 12-lead electrocardiogram (ECG) data, echocardiographic imaging and clinical history. A study found VFRisk to be more accurate than gauging risk based on LVEF alone.
“These 13 markers can all be obtained in a very inexpensive way from the electronic health record,” Chugh said. “And we can use machine learning and technology to automate it.”
Chugh’s follow-up study, the Observational Study of Sudden Cardiac Arrest Risk (OSCAR), is currently testing and refining the VFRisk algorithm in a population of roughly 400,000 Cedars-Sinai patients.
To improve the tool’s predictive accuracy, the team is harnessing the power of multimodal AI to combine and analyze data from additional biomarkers, including information from imaging, the genome, the proteome and biochemical markers in the blood.
Near-Term Prevention
In a 2016 study published in The Annals of Internal Medicine, Chugh discovered that many people experience warning symptoms in the days and weeks before a cardiac arrest, and these symptoms recur in the 24 hours before the event. Most people ignore their symptoms, but the 20% in the study who sought emergency care had a five- or six-fold higher chance of survival.
In a follow-up study, the team found symptoms differed by sex. For women, the most common symptom was shortness of breath, while men most commonly experienced chest pain.
Chugh’s team is further honing risk prediction for both sexes by combining warning symptoms reported by SCA survivors with their clinical profile.
“If this research is successful, our hope is that we can help a lot more people experiencing these warning symptoms avoid a cardiac arrest.”
AI and Heart Attacks
Investigators are also transforming how cardiologists predict the risk of myocardial infarction. The traditional approach has been to measure stenosis, or narrowing, of the arteries. But a team of Cedars-Sinai researchers led by Damini Dey, PhD, director of the Quantitative Imaging Analysis Program, has helped pivot the field toward measuring plaque itself, as opposed to just the narrowing it causes.
Using an FDA-approved software tool it developed called Autoplaque, which has been validated in more than 100 published studies, Dey’s team analyzes cardiac CT angiography (CCTA) images to quantify the more dangerous soft plaque as well as the more stable calcified plaque.
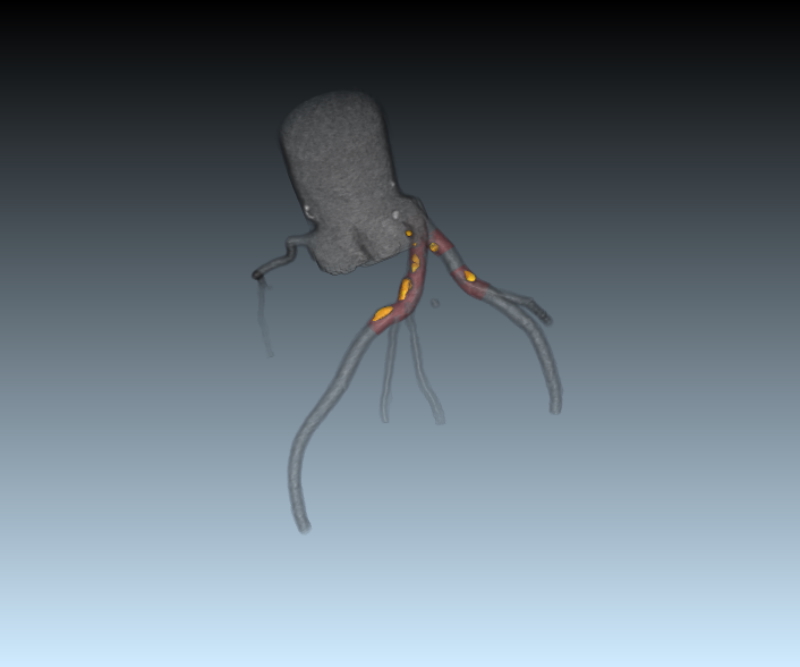
In a 2022 analysis of a multicenter trial published in The Lancet Digital Health, Dey’s team showed that plaque volume is a stronger predictor of MI than arterial stenosis.
“This really is a paradigm shift, because patients may appear healthy based on vessel narrowing alone, but they may actually be high risk due to the hidden buildup of plaque,” Dey said.
AI is a crucial component of the tool.
“Even for expert readers, plaque analysis is very time consuming,” Dey said. “They can be in the loop, but it wouldn’t be clinically feasible to measure the coronary plaque in all these scans without AI.”
Clinicians can use these more efficient and noninvasive risk assessments to tailor preventive therapies to reduce noncalcified plaque. Beginning next year, plaque measurement will be covered by some insurance plans, an important step toward broad clinical adoption.
Gleaning New Information From Existing Scans
In a 2024 study published in the journal Nature Communications, the research team of Piotr Slomka, PhD, director of Innovation in Imaging at Cedars-Sinai, demonstrated that in 18 seconds, an AI model could uncover valuable insights into heart health using simple CT scans, including measurements that previously have required the use of contrast or invasive procedures.
The tool is particularly useful in interpreting a noncontrast CT scan that accompanies a positron emission tomography (PET) scan, which visualizes tissues and organs using a radioactive tracer to monitor heart disease, cancer and other conditions. Traditionally, the CT scan’s only utility is to correct ambiguities in the more detailed PET scan.
“We've found a way to repurpose this correction scan to measure coronary calcium, epicardial adipose tissue, chamber volume, body composition and other biomarkers linked to cardiac risk,” said Slomka. “Now we want to see how well we can predict heart disease and cardiovascular death when compared with the gold-standard invasive tests using catheters.”
Slomka points out that this data can also be captured from other CT scans that include the entire chest, such as lung scans, allowing AI to analyze cardiac health as a byproduct whenever such a scan is taken.
“Cardiologists often order one test and look at one particular measure, such as perfusion or ejection fraction, and use that to guide treatment,” said Slomka. “What we are trying to do is take the holistic information in the image, process it automatically with AI and find many more features than can be extracted by hand. Based on all that information, we try to optimize predicting the risks to a patient’s heart health.”