Healing the Heart With Every Step
Date
February 18, 2026
Credits
Date
February 18, 2026
Credits
Medical providers featured in this article

In Brief
In fall 2024, Maria Dondero was driving across the Benicia-Martinez Bridge near her Napa Valley home when she felt her heart race aggressively. A strange tension built in her chest, as if it was being clenched, and she couldn’t catch her breath. She swerved her car off the road and dialed 911.
Moments later, paramedics arrived, and soon she was on oxygen at a nearby emergency room, where doctors determined the source of the terrifying episode: ventricular tachycardia (VT). VTs are bursts of three or more severely rapid beats from the lower heart that may hurt or interfere with breathing.
The arrythmias are especially life-threatening in patients like Dondero, who was diagnosed 35 years ago with mitral valve prolapse and regurgitation, heart disease causing pumping blood to flow backward and away from critical organs. Untreated, VTs, at a speed of 100 per minute, can lead to heart failure and sudden death.
{{cta-block}}
Seeking Cardiac Care Direction
By the time Maria ended up in the emergency department, her heart had sustained a lifetime of love: four decades of a deeply supportive marriage to her husband, Larry, two close adult daughters and her first grandchild. She also had enjoyed a rewarding career healing others as a pharmacist.
Until her new diagnosis, she’d relished exploring the rolling trails of California’s wine country with Larry and their chocolate lab. With corporate life in the empty nesters’ rearview, she’d nurtured cabernet grapes to fruition on the couple’s vineyard. But just as Dondero settled into this sweet, new season, she worried that freedom was slipping away.
For about six months after the scare on the bridge, the dizzy spells and unsteadiness worsened. She developed more intense, frequent premature ventricular contractions (PVCs) which, alongside the surging heart flutters she felt on the bridge, sent her cardiovascular system into a tailspin. These erratic heartbeats happen when electrical messages that prompt heart muscles to tighten rush ahead and misfire from the wrong place.
The frustrating symptoms gradually wore on Dondero, who was used to keeping up with their 8 acres, her toddler granddaughter, Aleia, and budding friendships in the tight-knit community.
Dondero’s longtime cardiologist told her that to fix her heart issues and restore healthy bloodflow, she would need mitral valve surgery.
“I was scared out of my mind,” she said. “I had no idea how I was going to get through this."
Dondero then met with a surgeon in nearby San Francisco, where the doctor seemed to talk at her, not with her. After exhaustive testing, he rattled off a list of problems—including a separate leak in her heart’s tricuspid valve she wasn’t aware of—and major procedures she may or may not need, such as a pacemaker implant.
“The experience was so overwhelming,” she said. “He just hit me with all of these issues and curveballs, and I couldn’t absorb it.”
Virtual Second Opinion: A Lifeline for Maria’s Heart
The prospect of undergoing extensive cardiac surgery left the Bay Area native frightened and unsure of where to turn. She wanted to verify that mitral valve operation was the best treatment course and would be enough to fix the condition.
Through Cedars-Sinai’s Virtual Second Opinion program, Joanna Chikwe, MD, chair of the Cedars-Sinai Department of Cardiac Surgery, reviewed Dondero’s medical records and provided a second opinion report on her care options, confirming the approach. The Virtual Second Opinion program enabled Dondero to secure review by a specialist from the comfort of her home and gave her the confidence to proceed with treatment.
“It’s your health, your life, and sometimes you don’t get a second chance.”
With her newfound assurance, the lifelong Californian jumped headlong into researching the highest-quality heart valve surgery programs across the U.S., hoping to find a medical team with the expertise to steady her heart.
“Maria’s valve condition is among the most common heart diagnoses, but it’s rare for a heart to leak so badly that it requires surgery,” said Chikwe, a worldwide leader in innovative surgical approaches.
Since mitral valve repair is highly specialized, many patients aren’t treated until they suffer severe damage, leading to heart failure, strokes and even death. As many as 50% of people who could benefit from repairing the degenerative, dangerous overflow don’t undergo surgery, despite its potential to restore normal life expectancy and quality of life. And a high number of patients who need a repair get less beneficial artificial valve replacements instead, according to an analysis of 2020 Medicare data. Robotic approaches are even harder to access.
“About half of robotic mitral surgery programs shut down after treating just a handful of patients, because of poor outcomes,” said Chikwe. “The chances of getting a good repair can be as low as 50%, whereas at Cedars-Sinai, we repair more than 99% of valves like Maria’s.”
A Surgical Solution to Severe Mitral Valve Disease
Dondero’s extensive search led her to decide on Cedars-Sinai’s Smidt Heart Institute for care. The Cardiac Surgery Program is at the forefront of robotic minimally invasive mitral valve repair, with a near-perfect success rate across more than 1,700 procedures. She also selected Chikwe as her surgeon.
“It’s your health, your life,” Dondero said, “and sometimes you don’t get a second chance.”
Chikwe evaluated Dondero at Cedars-Sinai and deduced that the best approach was to repair the mitral valve. This could resolve both leaks and Maria’s faulty heart rhythm all at once, steadying its beats without further unnecessary surgery. The gentler, safer plan also speeds up recovery.
For 90% to 95% of patients, this mend will last a lifetime.
Listening to the Heart
Dondero sought solace in meditative breathing, counting down each beat and day until her surgery just one month later. After establishing care with Cedars-Sinai, she and her heart surgery team held frequent, in-depth conversations that put her at ease.
“They exuded confidence, and that helped me feel good about where I was going and what I was doing,” she said.
Chikwe’s secret to connection: She listens.
“I ask a very simple, open-ended question: ‘How can we be helpful?’” she said. “People will tell you what they need.”
{{providers}}
Robotic Mitral Valve Repair, Powered by Human Relationships
During Maria’s surgery, Chikwe guided a DaVinci robot to make a credit card-sized cut at her side. Rather than the traditional route through the breastbone, she moved up a smoother path between the patient’s ribs to the heart. The heart is temporarily stopped to secure the valve, by reattaching torn cords or reinforcing loose flaps that cause it to prolapse.
This complex procedure demands close coordination across an experienced team of surgeons and critical care and anesthesiology specialists. With a tiny, high-resolution camera, they precisely tailored each incision and vigilantly monitored the patient for rare, potential surgical complications, including stroke and atrial fibrillation.
Chikwe, operating the robot, deftly closed Maria’s wounds with sutures thinner than a strand of hair.
In the skilled surgeon’s hands, the entire process took about 2.5 hours, and Dondero was cleared for discharge four days later.

A Steady Pace to Recovery
As Dondero underwent valve repair, flames from the Eaton and Palisades wildfires engulfed Los Angeles—but her medical team saw the repair through.
“It was really important to Maria to be able to get back to walking up and down the rows of vineyards and living life to the fullest,” Chikwe said. “She's living her dream, and it was wonderful to support her getting back to that.”
After the procedure, physical therapists demonstrated adaptive stretches and exercises to help her heal. When she left the hospital, the smoky L.A. air made it unsafe to walk outdoors—so she and Larry drove east.
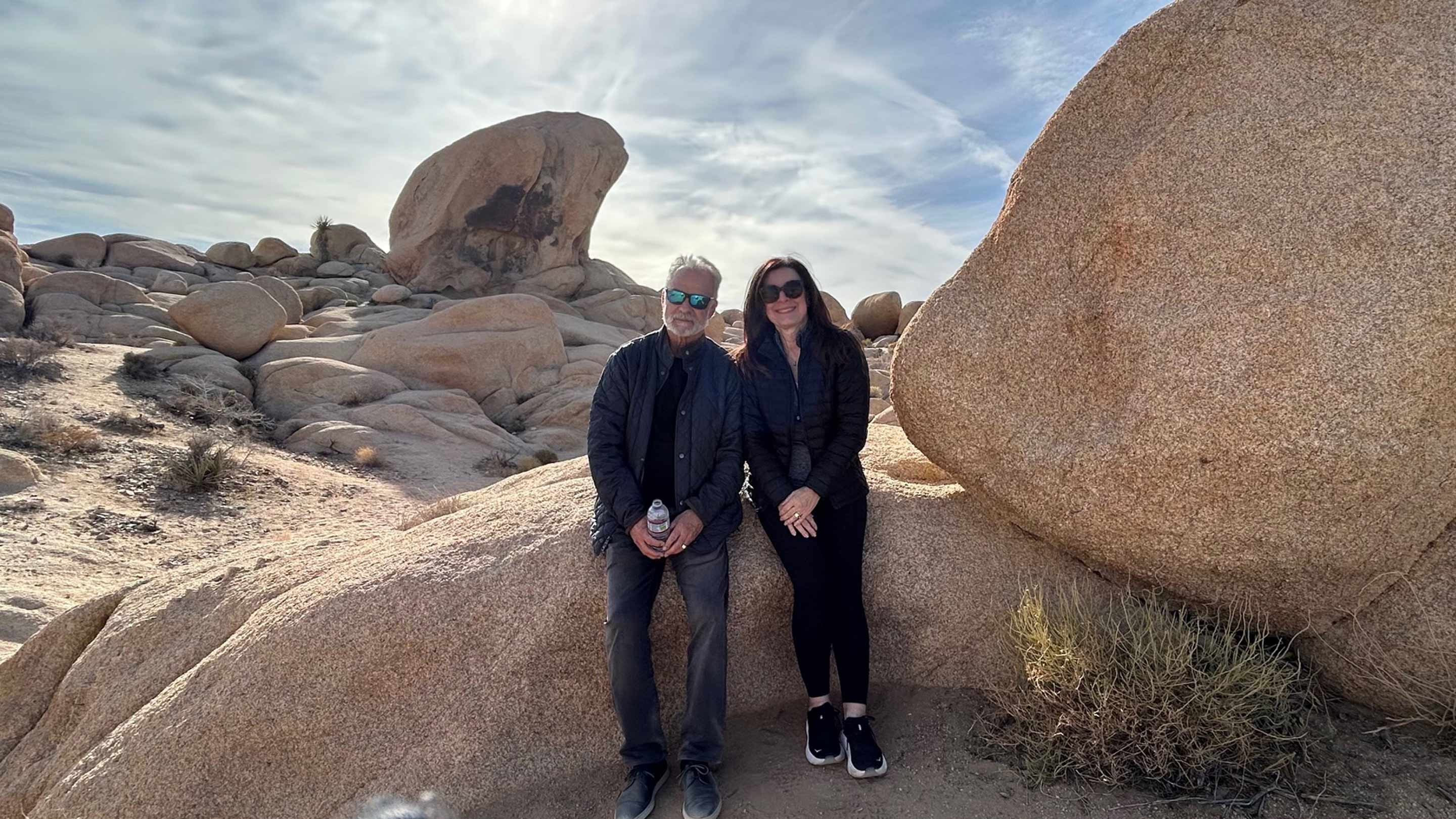
Under the clear skies of Joshua Tree National Park, a little sore and stiff but in awe of the unfolding desert beauty, Dondero reached the rocky summit of a mile-long hike. Six months later, she was amazed to find herself climbing the steep stairs that cut along the Western coast of Italy.
The challenges revitalized her. Dondero, grounded in family, savored the holidays with her daughters and granddaughter and is now back to walking neighboring footpaths dotted by wineries and grazing goats.
“I’m just so grateful,” she said. “I was able to go to a great place like Cedars-Sinai to have a smooth surgery, recover quickly and then enjoy my life as it had always been.”
Frequently Asked Questions
What is ventricular tachycardia (VT)?
VT is when the heart’s lower left compartment (ventricle) suddenly pumps too fast, beating three or more times in a row, at a pace of over 100 beats per minute. This flurry triggers palpitations, as well as chest pressure or pain, dizziness, shortness of breath and sometimes fainting.
Why are VTs a potentially serious complication for people with existing heart disease?
VTs are a leading cause of cardiac arrest. They are also behind many medical emergencies such as stroke, high blood pressure in the lungs, infections, heart failure—and even sudden death.
Why should patients with severe mitral valve disease get mitral valve repair surgery?
The mitral valve is essential to propelling blood in the right direction. Correcting a serious leak or damage reduces arrhythmias and can improve survival by up to 70%.
Will a mitral valve repair require further surgery?
As many as 90% to 95% of patients who have a robotic mitral valve repair don’t need another repair or replacement. Expert surgeons can safely close the valve and fix your heart for good.




