Cedars-Sinai Researchers Target Liver Disease and Cancer
Date
January 2, 2026
Credits
Date
January 2, 2026
Credits
Medical providers featured in this article


In Brief
Roughly one-third of adults in the U.S. have metabolic dysfunction-associated steatotic liver disease (MASLD)—previously known as nonalcoholic fatty liver disease.
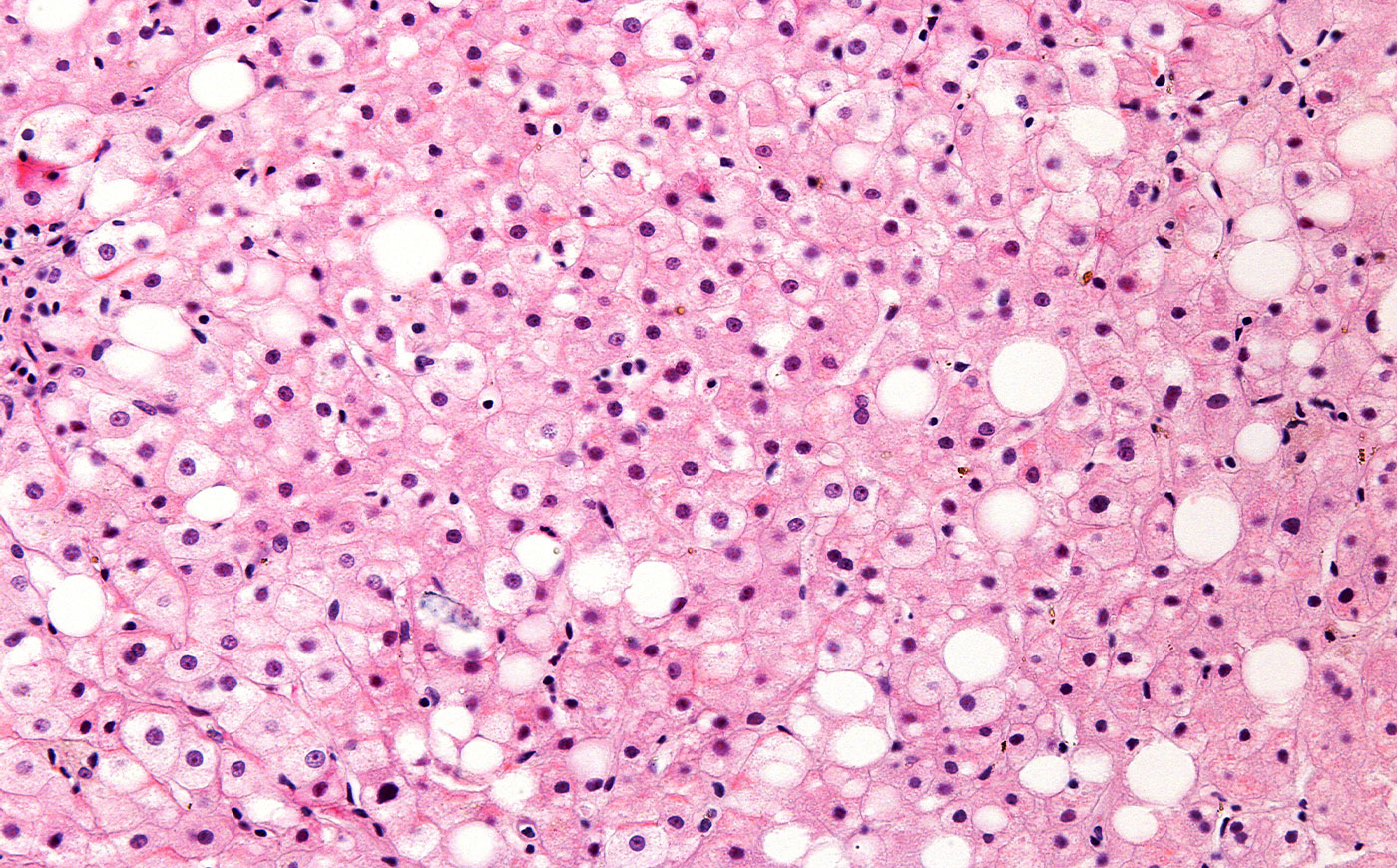
MASLD is caused by a buildup of fat in the liver. Its more advanced form, metabolic dysfunction-associated steatohepatitis (MASH), is when this fat buildup causes liver inflammation. Both MASLD and MASH are linked to a greater risk of developing liver cancer and cancer metastasis, which is when cancer spreads to other areas of the body.
The fat buildup and inflammation in the liver that are associated with MASLD and MASH, along with the scar tissue development they cause, can lead to mutations in liver cells that cause cancer, said Ju Dong Yang, MD, medical director of the Liver Cancer Program at Cedars-Sinai Cancer.
“It’s a perfect environment for cancer cells to develop,” he said.
According to some estimates, roughly 11,000 new cases of liver cancer related to MASLD and MASH are diagnosed each year. These diagnoses contribute to the global death toll from liver cancer, which is projected to double by 2050, according to a recent study in The Lancet.
MASLD and MASH have lagged behind other metabolic diseases, such as diabetes, in terms of diagnosis and treatment. However, recent years have brought breakthroughs for MASLD and MASH, including two approved medications for treating MASH.
“I cannot emphasize enough how important it is to improve the fatty liver to reduce the risk of cancer.”
At Cedars-Sinai, researchers are working to tackle these conditions from multiple angles. Here, we discuss three ways our experts are boosting diagnosis rates, uncovering new treatments and helping patients with liver disease reduce their risk for developing cancer. Our experts also offer practical tips for reducing your risk for—or reversing—liver disease.
Using AI to Uncover Liver Disease
The vast majority of patients with metabolic dysfunction-associated steatotic liver disease (MASLD) experience no symptoms from the condition. Plus, cases of MASLD are underdiagnosed, even though better screening would help prevent complications and reduce the likelihood of progression to metabolic dysfunction-associated steatohepatitis (MASH) and cancer.
But MASLD diagnosis isn’t straightforward, and someone with the condition can still have normal bloodwork. It typically takes a liver ultrasound to discover the fat accumulation associated with MASLD, and more advanced imaging to detect inflammation or scarring.
Earlier this year, Cedars-Sinai investigators uncovered a surprising new tool for diagnosing MASLD. Cardiologists in the Smidt Heart Institute at Cedars-Sinai designed an AI program that can identify chronic liver disease from videos taken during an echocardiogram, a common screening test for heart disease.
“Incorporating AI into echocardiograms, which capture images of the heart and the liver, can lead to a diagnosis of liver disease without additional costs,” said Alan Kwan, MD, assistant professor of Cardiology in the Smidt Heart Institute and senior and corresponding author of the study, published in NEJM AI.
Expanding Therapies for MASLD and MASH
Even when a patient is found to have MASLD, the diagnosis is often ignored or minimized, even though it can progress to MASH or cancer, said Shelly Lu, MD, director of the Karsh Division of Gastroenterology and Hepatology and the Women’s Guild Chair in Gastroenterology at Cedars-Sinai. She noted there is still low awareness of the risks of liver disease, and until recently, the only treatments were lifestyle modification and weight loss.
A breakthrough came in 2024 when the U.S. Food and Drug Administration (FDA) approved resmetirom (Rezdiffra) for use in treating patients with MASH. In 2025, the GLP-1 drug semaglutide (Wegovy) became the second FDA-approved medication for treating MASH. While these new drugs are great news for patients with MASH, it is unclear whether these drugs will lower the risk of liver cancer in these patients, Lu said.
There are currently no FDA-approved medications for patients with MASH that has progressed to liver cirrhosis, a progression that can lead to cancer or death. However, there are many new drugs in the pipeline. “I’m confident that in the next three to five years, we will have 10 or more medications that will be more tailored for specific groups of [liver disease] patients,” Yang said.
Studying the Potential for Over-the-Counter Treatment
Levels of S-adenosylmethionine (SAMe), a molecule that occurs naturally in the body and is available as an over-the-counter supplement, tend to decline in patients with liver disease. In fact, nearly half of all patients with MASLD likely have reduced SAMe levels, Lu said. When SAMe is low, it can trigger liver inflammation and scarring and increase patients’ risk of developing cancer.
The Lu Laboratory has studied the molecule for more than 20 years and showed that mice with reduced SAMe levels spontaneously develop liver disease. Lu and others found that mice that received SAMe supplements had reduced rates of liver cancer and inflammation-induced colorectal cancer.
“One of my longstanding hypotheses is that SAMe is useful as a preventive agent against liver cancer,” she said. “Although there is abundant preclinical data, this has yet to be critically examined in humans.”
That is set to change early next year. Lu is participating in a clinical trial to examine the effect of SAMe supplements on the progression of disease in patients with MASH. Yang is the principal investigator. The study will enroll about 100 MASH patients, half of whom will receive SAMe and the other half a placebo. It will follow the patients’ disease progression for more than a year.
Yang has been recommending SAMe supplements to his MASH patients for years. Anecdotally, he has seen improvement in both liver disease progression and other symptoms, including joint pain, arthritis and even mood.
“My clinical experience and Dr. Lu’s extensive preclinical evidence motivated us to conduct this trial,” Yang said. “The SAMe trial is unique, and it’s a very exciting field that we are pioneering.”
How to Reduce Your Risk of Developing Liver Disease and Cancer
According to Yang, preventing—and reversing—MASLD starts with a healthy lifestyle, including getting regular exercise and eating a healthy diet, such as the Mediterranean diet.
He also noted metabolic syndrome is likely a main driver of cancer in patients with MASLD. It’s important for patients to control risk factors for the condition, such as diabetes and high cholesterol.
“I cannot emphasize enough how important it is to improve the fatty liver to reduce the risk of cancer,” Yang said. “We, as physician-scientists, continue to investigate the risk factors we can work on to reduce the risk of future cancer development.”
Frequently Asked Questions
What are metabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH)?
MASLD is a condition caused by a buildup of fat in the liver. MASH is an advanced form of MASLD in which fat buildup in the liver causes liver inflammation.
What are the health risks associated with MASLD and MASH?
Both MASLD and MASH are linked to a greater risk of developing liver cancer and cancer metastasis, which is when cancer spreads to other areas of the body.
How are MASLD and MASH diagnosed?
Currently, liver ultrasound is the most effective tool for diagnosing MASLD. Other imaging modalities can diagnose inflammation and scarring. Cedars-Sinai researchers have also designed an AI program that can identify chronic liver disease from videos taken during an echocardiogram.
What treatments are available for MASLD and MASH?
Lifestyle modification and weight loss are the standard treatments for MASLD. Recently, the FDA approved two drugs, resmetirom and semaglutide, for treating MASH, and experts anticipate the development of drugs for treating MASLD in the future.
How can patients with MASLD reduce their risk for developing liver cancer?
Regular exercise and eating a healthy diet, such as a Mediterranean diet, can help prevent or reverse MASLD, thereby reducing cancer risk. Cedars-Sinai experts are also investigating whether S-adenosylmethionine (SAMe) supplements can slow disease progression and reduce cancer risk in patients with MASLD.






